Epithelial tissue is a cornerstone of animal anatomy, forming a critical barrier that lines both the external surfaces of the body and the internal cavities of organs. This tissue is essential for multicellular organisms, where specialized cells are organized into tissues, organs, and systems that work in harmony to perform vital functions such as protection, secretion, absorption, and sensory reception. Unlike unicellular organisms, where a single cell handles all life processes, multicellular organisms rely on epithelial tissue to execute specialized roles with remarkable precision.
This article provides an in-depth exploration of epithelial tissue, its characteristics, types, functions, and its indispensable role in maintaining bodily integrity.
Table of Contents
Understanding Epithelial Tissue
Epithelial tissue, often referred to as epithelium (from the Greek words epi, meaning “upon,” and thele, meaning “nipple”), is a fundamental type of animal tissue that covers surfaces, lines cavities, and forms glands. Composed of tightly packed cells with minimal intercellular matrix, epithelial tissue is supported by a non-cellular basement membrane that anchors it to underlying connective tissue. This tissue is unique in its lack of direct blood supply, relying instead on diffusion from nearby blood vessels for nutrients and oxygen. In some cases, epithelial tissues are innervated by nerve endings, enabling sensory functions.
Epithelial tissue is found throughout the body, from the skin’s outer layer to the linings of organs like the stomach, intestines, and lungs. Its versatility allows it to perform diverse roles, such as protecting underlying tissues, facilitating absorption, and enabling secretion. The close packing of cells and specialized intercellular junctions ensure that epithelial tissue acts as an effective barrier while allowing selective passage of materials.
Characteristics of Epithelial Tissue
Epithelial tissue is defined by several distinct characteristics that enable it to fulfill its diverse roles:
- Tight Cell Arrangement: Epithelial cells are densely packed with minimal intercellular spaces (20–30 nm wide), forming a continuous sheet that acts as a protective barrier.
- Intercellular Junctions: Specialized junctions, including tight junctions, adherens junctions, desmosomes, and gap junctions, connect adjacent cells, ensuring structural integrity and facilitating communication.
- Polarity: Epithelial cells exhibit bipolarity, with an apical surface facing the external environment or a body cavity and a basal surface attached to the basement membrane.
- Basement Membrane Support: The non-cellular basement membrane provides structural support and anchors epithelial tissue to underlying connective tissue.
- Avascularity: Epithelial tissue lacks its own blood supply, relying on diffusion for nourishment.
- Innervation: Some epithelial tissues are innervated, allowing them to serve sensory functions, such as in the skin or olfactory epithelium.
- Regeneration: Epithelial cells have a high regenerative capacity, enabling rapid replacement of damaged or worn cells, particularly in areas subject to friction, like the skin or intestinal lining.
These characteristics make epithelial tissue uniquely suited to its protective, absorptive, and secretory roles.
Intercellular Junctions in Epithelial Tissue
The strength and functionality of epithelial tissue depend on specialized intercellular junctions that connect adjacent cells. These junctions ensure structural cohesion, regulate material passage, and facilitate communication. The primary types include:
- Tight Junctions: Found at the apical region, these junctions seal adjacent cells together, controlling the movement of substances between cells. They are critical in environments like the intestinal lining, where they prevent leakage of digestive contents.
- Adherens Junctions: These junctions, including desmosomes and hemidesmosomes, provide mechanical strength by anchoring cells to each other or to the basement membrane.
- Desmosomes: These act as strong anchors, particularly in tissues subject to mechanical stress, such as the skin.
- Gap Junctions: Formed by protein channels called connexins, gap junctions allow the passage of ions and small molecules between cells, enabling rapid communication. They are essential in tissues requiring coordinated activity, such as cardiac muscle.
These junctions collectively ensure that epithelial tissue functions as a cohesive, selective barrier.
Types of Epithelial Tissue
Epithelial tissue is broadly classified into three categories based on structure and function: simple epithelial tissue, compound epithelial tissue, and specialized epithelial tissue. Each type is further subdivided based on cell shape, arrangement, and specific adaptations.
Simple Epithelial Tissue
Simple epithelial tissue consists of a single layer of cells resting on a basement membrane. It is typically found in areas with minimal wear and tear, where functions like absorption, secretion, and diffusion are critical. The subtypes include:
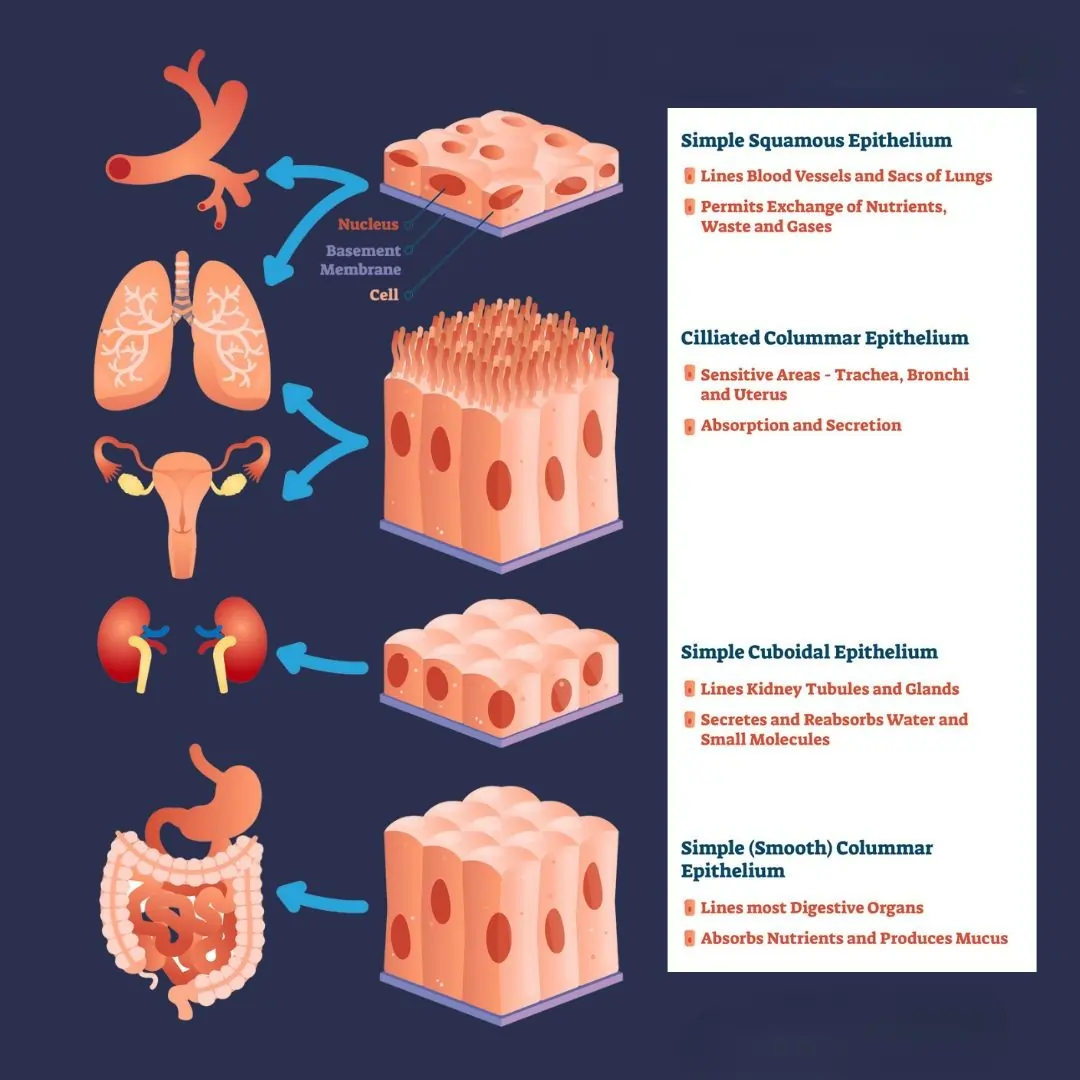
- Simple Squamous Epithelium: Composed of a single layer of flattened, polygonal cells, this epithelium resembles tiles on a floor, earning it the name pavement epithelium. Tight junctions hold the cells together, facilitating rapid diffusion. It is found in the alveoli of lungs, pericardial and abdominal cavities, and blood vessel linings, where it supports gaseous exchange, secretion, and fluid movement.
- Simple Cuboidal Epithelium: Made of cube-shaped cells with centrally located, spherical nuclei, this epithelium is found in glandular tissues and kidney tubules. Its microvilli (in some cases) increase surface area for absorption and secretion. Functions include urine formation in kidneys and gamete production in gonads.
- Simple Columnar Epithelium: This consists of tall, vertically aligned cells with elongated nuclei near the base. Some cells, known as goblet cells, secrete mucus. It lines the stomach, intestines, digestive glands, and gallbladder, supporting absorption and secretion.
- Simple Ciliated Epithelium: Characterized by cilia on the apical surface, this epithelium moves substances like mucus or particles in a specific direction. It is found in the respiratory tract, uterus, and testicular tubules. Subtypes include simple ciliated columnar epithelium (e.g., in the respiratory system) and simple ciliated cuboidal epithelium (e.g., in urinary tubules).
- Pseudostratified Epithelium: Despite appearing multilayered, this is a single-layered epithelium with nuclei at varying heights, giving a false stratified appearance. Subtypes include pseudostratified columnar epithelium (e.g., in salivary gland ducts) and pseudostratified ciliated columnar epithelium (e.g., in the trachea), which moves mucus and particles.
Compound Epithelial Tissue
Compound epithelial tissue, also known as stratified epithelium, consists of multiple cell layers, making it ideal for areas subject to significant wear and tear. It is divided into two main types:
- Stratified Squamous Epithelium: This has multiple layers, with the basal layer containing columnar or cuboidal cells that undergo mitosis to regenerate surface cells. It is further divided into:
- Keratinized Stratified Squamous Epithelium: Found in the epidermis of terrestrial vertebrates, this epithelium contains keratin, a tough, waterproof protein that protects against abrasion and dehydration.
- Non-Keratinized Stratified Squamous Epithelium: Lacking keratin, this type lines moist surfaces like the buccal cavity, esophagus, vagina, and cornea, providing protection without waterproofing.
- Stratified Cuboidal Epithelium: Comprising cuboidal cells in the outer layer and columnar cells in the basal layer, this is found in salivary glands, pancreatic ducts, and the epidermis of some amphibians.
- Stratified Columnar Epithelium: With columnar cells in both basal and surface layers, this rare epithelium lines parts of the urethra, mammary gland ducts, and epiglottis.
- Stratified Ciliated Columnar Epithelium: Featuring ciliated columnar cells on the surface, this lines the larynx and soft palate.
- Transitional Epithelium: A unique type of compound epithelium, transitional epithelium is elastic and less dense than stratified epithelium. It has cuboidal basal cells, polygonal or pear-shaped middle cells, and large, oval surface cells. Found in the urinary bladder, ureter, and renal pelvis, it stretches to accommodate fluid volume changes.
Specialized Epithelial Tissue
Specialized epithelial tissue is adapted for specific functions, such as secretion or sensory perception. Key types include:
- Glandular Epithelium: Composed of cells specialized for secretion, this is divided into:
- Unicellular Glandular Epithelium: Single cells, like goblet cells, secrete mucus in the alimentary canal.
- Multicellular Glandular Epithelium: Groups of cells form glands, such as salivary glands, for secretion.
- Germinal Epithelium: Found in testes and ovaries, this consists of cuboidal cells that produce gametes (sperm and ova).
- Sensory Epithelium: Containing neurosensory cells, this is found in the olfactory region, retina, and taste buds, enabling sensory perception.
- Pigmented Epithelium: Located in the retina, iris, and pigmented skin layers, this contains pigments like melanin to regulate light or provide coloration.
Functions of Epithelial Tissue
Epithelial tissue performs a wide array of functions critical to the body’s survival and homeostasis:
- Protection: Epithelial tissue shields underlying tissues from mechanical damage, pathogens, and dehydration. For example, keratinized stratified squamous epithelium in the skin prevents water loss and abrasion.
- Absorption: Simple columnar epithelium in the intestines absorbs nutrients, while simple cuboidal epithelium in kidney tubules reabsorbs water and ions.
- Secretion: Glandular epithelium produces substances like mucus, digestive enzymes, and hormones. Goblet cells secrete mucus to lubricate and protect surfaces.
- Sensory Reception: Sensory epithelium in the retina and taste buds detects light, chemicals, and other stimuli, transmitting signals to the nervous system.
- Gas Exchange: Simple squamous epithelium in the alveoli facilitates oxygen and carbon dioxide exchange between blood and air.
- Transport: Ciliated epithelium moves mucus, particles, or fluids along surfaces, as seen in the respiratory tract and fallopian tubes.
- Reproduction: Germinal epithelium produces gametes, ensuring the continuation of species.
- Exoskeletal Formation: Epithelial tissue contributes to structures like hair, nails, feathers, and scales, providing additional protection.
- Filtration: In nephrons, epithelial tissue filters blood to form urine, regulating body fluid composition.
Importance of Epithelial Tissue in Health and Disease
Epithelial tissue’s diverse roles make it critical to overall health. Its protective function prevents infections and injuries, while its absorptive and secretory roles support digestion, respiration, and homeostasis. However, disruptions in epithelial tissue can lead to significant health issues. For example, damage to the respiratory epithelium can impair mucus clearance, increasing infection risk. Abnormal growth of epithelial cells can lead to carcinomas, a common type of cancer originating in epithelial tissues, such as squamous cell carcinoma in the skin or adenocarcinoma in glandular tissues.
The regenerative capacity of epithelial tissue is vital for wound healing. For instance, the epidermis rapidly replaces damaged cells to restore the skin’s barrier function. In medical applications, epithelial tissue is studied for tissue engineering, where scientists aim to grow artificial epithelia for transplants or wound repair.
Table: Comparison of Epithelial Tissue Types
| Type | Structure | Location | Function |
|---|---|---|---|
| Simple Squamous Epithelium | Single layer of flattened cells | Alveoli, blood vessels, body cavities | Diffusion, secretion, gaseous exchange |
| Simple Cuboidal Epithelium | Single layer of cube-shaped cells | Kidney tubules, glands | Absorption, secretion, gamete production |
| Simple Columnar Epithelium | Single layer of tall, vertical cells | Stomach, intestines, gallbladder | Absorption, secretion, protection |
| Simple Ciliated Epithelium | Single layer with cilia | Respiratory tract, uterus, testes | Movement of mucus or particles |
| Pseudostratified Epithelium | Single layer, appears multilayered | Trachea, salivary glands, male urethra | Secretion, mucus transport |
| Stratified Squamous Epithelium | Multiple layers, surface cells flattened | Skin, esophagus, mouth, cornea | Protection against abrasion, pathogens |
| Stratified Cuboidal Epithelium | Multiple layers, surface cells cuboidal | Salivary glands, pancreatic ducts | Protection, secretion |
| Stratified Columnar Epithelium | Multiple layers, surface cells columnar | Urethra, mammary glands, epiglottis | Protection, secretion |
| Transitional Epithelium | Multiple elastic layers, variable shapes | Urinary bladder, ureter, renal pelvis | Stretching, protection |
| Glandular Epithelium | Specialized for secretion | Glands (e.g., salivary, goblet cells) | Secretion of mucus, enzymes, hormones |
| Sensory Epithelium | Contains neurosensory cells | Retina, olfactory region, taste buds | Sensory perception |
| Germinal Epithelium | Cuboidal cells for gamete production | Testes, ovaries | Gamete production |
Additional Insights into Epithelial Tissue
Recent research has highlighted the dynamic nature of epithelial tissue in responding to environmental changes. For example, epithelial-mesenchymal transition (EMT) is a process where epithelial cells transform into mesenchymal cells, gaining mobility and aiding in wound healing or embryonic development. However, EMT is also implicated in cancer metastasis, where epithelial tumor cells become invasive.
In biotechnology, epithelial tissue is a focus for developing organoids—miniature organ-like structures grown in vitro. These organoids, derived from epithelial stem cells, are used to study diseases, test drugs, and explore regenerative medicine. For instance, intestinal organoids help researchers understand digestive disorders like Crohn’s disease.
Epithelial tissue also plays a role in the immune system. Intraepithelial lymphocytes, immune cells embedded within epithelial layers, monitor for pathogens and initiate immune responses, particularly in the gut and skin. This underscores the epithelium’s role as both a physical and immunological barrier.
Conclusion
Epithelial tissue is a remarkable and versatile component of animal anatomy, serving as the body’s first line of defense and a key player in numerous physiological processes. From protecting against environmental hazards to facilitating nutrient absorption and sensory perception, its diverse types and functions are integral to life. Understanding the structure, characteristics, and roles of epithelial tissue not only deepens our appreciation of biological complexity but also informs medical advancements in tissue repair, cancer treatment, and regenerative medicine. As research continues to uncover the intricacies of epithelial tissue, its significance in health and disease remains undeniable, solidifying its status as a cornerstone of multicellular life.
Frequently Asked Questions (FAQs)
FAQ 1: What is epithelial tissue, and why is it important in the body?
Epithelial tissue, often referred to as epithelium, is a fundamental type of animal tissue that forms a protective layer covering the body’s external surfaces and lining internal organs and cavities. It consists of tightly packed cells with minimal intercellular matrix, supported by a non-cellular basement membrane. This tissue is essential for multicellular organisms, as it performs critical functions like protection, secretion, absorption, and sensory reception, distinguishing it from unicellular organisms where a single cell handles all processes.
The importance of epithelial tissue lies in its versatility. It acts as a barrier, shielding underlying tissues from physical damage, pathogens, and dehydration. For example, the keratinized stratified squamous epithelium in the skin prevents water loss and abrasion, while the simple squamous epithelium in the lungs facilitates gas exchange. Additionally, epithelial tissue contributes to physiological processes like nutrient absorption in the intestines and mucus secretion in the respiratory tract. Its high regenerative capacity ensures rapid repair of damaged surfaces, such as in wound healing, making it indispensable for maintaining bodily integrity and homeostasis.
FAQ 2: What are the main characteristics of epithelial tissue?
Epithelial tissue is defined by several distinct characteristics that enable it to perform its diverse roles effectively. These features ensure that epithelial cells work as a cohesive unit to protect, absorb, secrete, or sense stimuli. The tissue’s unique structure is tailored to its location and function in the body.
Key characteristics include:
- Tight Cell Arrangement: Epithelial cells are closely packed with minimal intercellular gaps (20–30 nm), forming a continuous sheet that acts as a barrier.
- Intercellular Junctions: Structures like tight junctions, adherens junctions, desmosomes, and gap junctions connect cells, ensuring structural integrity and facilitating communication.
- Polarity: Epithelial cells have an apical surface facing the external environment or a cavity and a basal surface attached to the basement membrane.
- Avascularity: Lacking blood vessels, epithelial tissue relies on diffusion for nutrients and oxygen.
- Regeneration: Epithelial cells have a high turnover rate, allowing rapid replacement of damaged cells, as seen in the skin or intestinal lining.
For instance, the simple columnar epithelium in the intestines uses its polarity and microvilli to maximize nutrient absorption, while tight junctions prevent leakage of digestive contents. These characteristics make epithelial tissue adaptable to various physiological demands.
FAQ 3: What are the different types of epithelial tissue?
Epithelial tissue is broadly classified into three categories: simple epithelial tissue, compound epithelial tissue, and specialized epithelial tissue. Each type is further subdivided based on cell shape, arrangement, and function, allowing epithelial tissue to meet the body’s diverse needs.
Simple epithelial tissue consists of a single layer of cells and is found in areas with minimal wear, such as the alveoli (simple squamous), kidney tubules (simple cuboidal), intestines (simple columnar), and respiratory tract (simple ciliated). Pseudostratified epithelium, despite appearing multilayered, is also a single-layered tissue found in the trachea. Compound epithelial tissue, or stratified epithelium, has multiple layers and is suited for high-friction areas like the skin (stratified squamous) or urinary bladder (transitional). Specialized epithelial tissue includes glandular epithelium (e.g., salivary glands), sensory epithelium (e.g., retina), and germinal epithelium (e.g., testes).
Each type is tailored to its function. For example, transitional epithelium in the bladder stretches to accommodate urine, while glandular epithelium in goblet cells secretes mucus to protect the intestinal lining. This diversity ensures epithelial tissue supports various physiological roles.
FAQ 4: How do intercellular junctions contribute to epithelial tissue function?
Intercellular junctions are specialized structures that connect epithelial cells, ensuring structural cohesion, selective permeability, and communication. These junctions are critical for maintaining the integrity of epithelial tissue as a barrier and facilitating its functions in protection, absorption, and secretion.
The main types of junctions include:
- Tight Junctions: These seal adjacent cells at the apical surface, controlling the passage of materials. For example, in the intestinal lining, tight junctions prevent harmful substances from leaking into the bloodstream.
- Adherens Junctions: Including desmosomes and hemidesmosomes, these provide mechanical strength by anchoring cells to each other or the basement membrane. Desmosomes are vital in the skin, resisting mechanical stress.
- Gap Junctions: Formed by connexin proteins, these create channels for the exchange of ions and small molecules, enabling rapid communication. In the heart, gap junctions coordinate muscle contractions.
These junctions work together to ensure epithelial tissue functions effectively. For instance, in the simple squamous epithelium of blood vessels, tight junctions maintain vascular integrity, while gap junctions in glandular tissues coordinate secretion.
FAQ 5: What is the role of simple epithelial tissue in the body?
Simple epithelial tissue, characterized by a single layer of cells resting on a basement membrane, is found in areas requiring efficient absorption, secretion, or diffusion with minimal friction. Its thin structure makes it ideal for facilitating rapid material exchange while providing a protective lining.
The subtypes of simple epithelial tissue serve distinct roles:
- Simple Squamous Epithelium: Found in the alveoli and blood vessels, it supports gaseous exchange and fluid secretion due to its thin, flattened cells.
- Simple Cuboidal Epithelium: Located in kidney tubules and glands, it facilitates absorption, secretion, and gamete production, often enhanced by microvilli.
- Simple Columnar Epithelium: Present in the intestines and stomach, it absorbs nutrients and secretes mucus via goblet cells.
- Simple Ciliated Epithelium: Found in the respiratory tract and fallopian tubes, its cilia move mucus or reproductive cells.
- Pseudostratified Epithelium: In the trachea, it transports mucus and particles, protecting the respiratory system.
For example, the simple columnar epithelium in the small intestine maximizes nutrient absorption, while ciliated epithelium in the trachea clears dust and pathogens, highlighting the tissue’s critical role in maintaining bodily functions.
FAQ 6: How does compound epithelial tissue differ from simple epithelial tissue?
Compound epithelial tissue, also known as stratified epithelium, consists of multiple layers of cells, making it more robust than simple epithelial tissue, which has a single layer. This structural difference allows compound epithelium to withstand greater mechanical stress and wear, making it ideal for high-friction areas, while simple epithelium is suited for absorption and diffusion.
Compound epithelial tissue includes:
- Stratified Squamous Epithelium: Found in the skin (keratinized) and esophagus (non-keratinized), it protects against abrasion and pathogens.
- Stratified Cuboidal Epithelium: Present in salivary glands, it supports secretion and protection.
- Stratified Columnar Epithelium: Found in the urethra, it provides structural support.
- Transitional Epithelium: Located in the urinary bladder, it stretches to accommodate fluid volume changes.
In contrast, simple epithelial tissue (e.g., simple squamous in alveoli) is thinner and facilitates rapid exchange. For example, the stratified squamous epithelium in the skin regenerates via mitosis in the basal layer to replace worn cells, while simple columnar epithelium in the intestines focuses on nutrient absorption. The choice of tissue type depends on the location and functional demands.
FAQ 7: What is the significance of specialized epithelial tissue?
Specialized epithelial tissue is adapted to perform specific functions, such as secretion, sensory perception, or gamete production, making it critical for targeted physiological roles. Unlike general epithelial tissues, which focus on protection or absorption, specialized types have unique structures tailored to their tasks.
Key types include:
- Glandular Epithelium: Comprising unicellular (e.g., goblet cells) or multicellular (e.g., salivary glands) forms, it secretes mucus, hormones, or enzymes. For instance, goblet cells in the intestines produce mucus to protect the lining.
- Sensory Epithelium: Found in the retina or olfactory region, it contains neurosensory cells that detect light or odors, transmitting signals to the brain.
- Germinal Epithelium: Located in the testes and ovaries, it produces gametes (sperm and ova), essential for reproduction.
- Pigmented Epithelium: Present in the retina, it regulates light absorption to enhance vision.
These specialized tissues enhance the body’s ability to interact with its environment and maintain reproductive and sensory functions. For example, the sensory epithelium in taste buds allows perception of flavors, while germinal epithelium ensures species continuity.
FAQ 8: How does epithelial tissue contribute to protection in the body?
Epithelial tissue serves as the body’s primary protective barrier, shielding underlying tissues from mechanical damage, pathogens, and dehydration. Its tightly packed cells and intercellular junctions create a formidable defense, while its regenerative capacity ensures rapid repair of damaged areas.
Specific protective roles include:
- Physical Barrier: Keratinized stratified squamous epithelium in the skin, rich in keratin, prevents water loss and resists abrasions, as seen in terrestrial vertebrates.
- Pathogen Defense: Tight junctions in the intestinal epithelium block harmful microbes, while ciliated epithelium in the trachea moves mucus-trapped pathogens out of the respiratory system.
- Chemical Protection: Goblet cells in the respiratory and digestive tracts secrete mucus to trap and neutralize harmful substances.
- Regeneration: The high turnover rate of epithelial cells, such as in the epidermis, ensures quick replacement of damaged cells, maintaining the barrier.
For example, the non-keratinized stratified squamous epithelium in the mouth protects against friction from chewing, while transitional epithelium in the bladder safeguards against urine’s chemical effects. These mechanisms collectively ensure robust protection.
FAQ 9: How does epithelial tissue support absorption and secretion?
Epithelial tissue plays a vital role in absorption and secretion, facilitating the uptake of nutrients and the release of substances like mucus, enzymes, and hormones. Its structure, including microvilli and goblet cells, is optimized for these processes in various organs.
In absorption, simple columnar epithelium in the small intestine uses microvilli to increase surface area, efficiently absorbing nutrients like glucose and amino acids. Similarly, simple cuboidal epithelium in kidney tubules reabsorbs water and ions during urine formation. For secretion, glandular epithelium is key. Unicellular glandular epithelium, like goblet cells, secretes mucus to lubricate the digestive tract, while multicellular glandular epithelium in salivary glands produces saliva containing digestive enzymes.
For example, in the stomach, simple columnar epithelium secretes mucus to protect the lining from acidic gastric juices, while absorbing certain drugs or ions. These functions are critical for digestion, waste elimination, and maintaining fluid balance, highlighting epithelial tissue’s role in homeostasis.
FAQ 10: What is the role of epithelial tissue in disease and medical research?
Epithelial tissue is central to both health and disease, as its dysfunction can lead to various conditions, particularly carcinomas—cancers originating from epithelial cells. Its regenerative and structural properties also make it a focal point in medical research, especially in tissue engineering and regenerative medicine.
In disease, damage to epithelial tissue can impair its protective or functional roles. For instance, chronic damage to the respiratory epithelium from smoking can disrupt mucus clearance, increasing infection risk. Abnormal epithelial cell growth can lead to cancers like squamous cell carcinoma (skin) or adenocarcinoma (glands). The epithelial-mesenchymal transition (EMT), where epithelial cells gain mobility, is implicated in cancer metastasis, allowing tumors to spread.
In research, epithelial tissue is studied for its regenerative potential. Scientists use epithelial stem cells to create organoids, miniature organ-like structures, to study diseases like Crohn’s or test drugs. For example, intestinal organoids help explore digestive disorders. Additionally, intraepithelial lymphocytes within epithelial layers are investigated for their role in immune defense, particularly in the gut. These advancements underscore epithelial tissue’s significance in developing treatments for cancer, wounds, and organ repair.
FAQ 11: How does the structure of epithelial tissue support its functions?
Epithelial tissue is uniquely structured to perform its diverse roles, such as protection, absorption, secretion, and sensory reception. Its tightly packed cells, minimal intercellular matrix, and support from a basement membrane create a versatile framework that adapts to specific physiological needs. The tissue’s design ensures it can act as a barrier, facilitate material exchange, and maintain structural integrity across various body surfaces.
Key structural features include:
- Close Cell Packing: The minimal intercellular spaces (20–30 nm) form a continuous sheet, ideal for protection, as seen in the keratinized stratified squamous epithelium of the skin.
- Polarity: The apical surface faces external or internal environments, while the basal surface anchors to the basement membrane, enabling directional functions like absorption in the simple columnar epithelium of the intestines.
- Intercellular Junctions: Tight junctions, desmosomes, and gap junctions ensure cohesion and selective permeability, critical in the simple squamous epithelium of blood vessels for preventing leaks.
- Avascularity: Lacking blood vessels, epithelial tissue relies on diffusion, which supports its thin structure for diffusion in the alveoli.
- Regenerative Capacity: High cell turnover, as in the epidermis, allows rapid repair of damaged surfaces.
For example, the simple ciliated epithelium in the respiratory tract uses cilia on its apical surface to move mucus, while its tight junctions prevent pathogen infiltration. This structural adaptability makes epithelial tissue essential for maintaining bodily functions.
FAQ 12: What role does the basement membrane play in epithelial tissue?
The basement membrane is a thin, non-cellular layer that anchors epithelial tissue to underlying connective tissue, providing structural support and regulating cellular functions. Composed of proteins like collagen and laminin, it acts as a scaffold that maintains tissue integrity and facilitates communication between epithelial and connective tissues.
The basement membrane’s roles include:
- Anchoring: It secures epithelial cells via hemidesmosomes, preventing detachment, as seen in the stratified squamous epithelium of the skin.
- Selective Filtration: It regulates the passage of nutrients and signaling molecules from connective tissue to epithelial cells, critical for the avascular nature of epithelium.
- Cell Differentiation: The basement membrane influences cell behavior, guiding regeneration and repair, as in wound healing in the epidermis.
- Barrier Function: It restricts the movement of large molecules or pathogens, enhancing the protective role of epithelial tissue.
For instance, in the simple squamous epithelium of the glomerulus in kidneys, the basement membrane filters blood to form urine while preventing protein loss. Damage to the basement membrane, as in certain kidney diseases, can impair filtration, highlighting its critical role in epithelial function.
FAQ 13: Why is epithelial tissue considered avascular, and how does it receive nutrients?
Epithelial tissue is described as avascular because it lacks its own blood vessels, a characteristic that distinguishes it from other tissues like connective tissue. This absence of direct blood supply is due to the tissue’s tightly packed cells and thin structure, which are optimized for functions like diffusion, protection, and secretion rather than housing vascular networks.
Instead of blood vessels, epithelial tissue relies on diffusion from underlying connective tissue, which contains blood vessels, to obtain nutrients and oxygen. The basement membrane facilitates this process by allowing small molecules to pass from the connective tissue to epithelial cells. The efficiency of diffusion depends on the tissue’s thickness; for example, the simple squamous epithelium in the alveoli is extremely thin, enabling rapid gas exchange. In contrast, thicker stratified epithelium, like in the skin, relies on diffusion from deeper layers, supported by its regenerative basal cells.
This avascular nature is advantageous for maintaining a compact barrier, as seen in the simple columnar epithelium of the intestines, where nutrient absorption occurs without interference from blood vessels. However, it also makes epithelial tissue vulnerable to damage if the underlying connective tissue’s blood supply is compromised, as in chronic wounds.
FAQ 14: How does ciliated epithelium function in the body?
Ciliated epithelium, a subtype of simple epithelial tissue, is characterized by hair-like projections called cilia on its apical surface. These cilia move in coordinated waves to transport substances like mucus, particles, or fluids across the epithelial surface, playing a vital role in maintaining organ function and protecting against pathogens.
The functions of ciliated epithelium include:
- Mucus Transport: In the respiratory tract, simple ciliated columnar epithelium moves mucus containing trapped dust and microbes toward the throat for expulsion, protecting the lungs.
- Fluid Movement: In the fallopian tubes, ciliated epithelium aids in transporting the ovum toward the uterus, supporting reproduction.
- Particle Clearance: In the trachea, pseudostratified ciliated columnar epithelium clears inhaled particles, preventing respiratory infections.
- Sensory Support: In some cases, cilia detect environmental changes, as in the ependymal cells of the brain’s ventricles.
For example, damage to the ciliated epithelium from smoking can impair mucus clearance, leading to chronic bronchitis. The synchronized beating of cilia, powered by cellular energy, ensures efficient movement, making this tissue critical for respiratory and reproductive health.
FAQ 15: What is the difference between keratinized and non-keratinized stratified squamous epithelium?
Stratified squamous epithelium is a type of compound epithelial tissue with multiple cell layers, designed to protect against abrasion. It is divided into keratinized and non-keratinized types, which differ in structure, function, and location based on the presence or absence of keratin, a tough, waterproof protein.
Keratinized stratified squamous epithelium contains keratin, which forms a hard, protective layer on the surface. Found in the epidermis of the skin in terrestrial vertebrates, it prevents water loss, resists mechanical damage, and blocks pathogen entry. The surface cells are dead and filled with keratin, forming a durable barrier, as seen in areas prone to friction like the palms. Non-keratinized stratified squamous epithelium, lacking keratin, remains moist and flexible. It lines areas like the mouth, esophagus, vagina, and cornea, providing protection without waterproofing, suitable for wet environments.
For instance, the keratinized epithelium of the skin protects against sunburn and abrasions, while the non-keratinized epithelium in the mouth withstands chewing without drying out. These differences ensure each type is adapted to its specific environment and functional demands.
FAQ 16: How does transitional epithelium function in the urinary system?
Transitional epithelium, a specialized type of compound epithelial tissue, is uniquely adapted to line organs of the urinary system, such as the urinary bladder, ureter, and renal pelvis. Its elastic and multilayered structure allows it to stretch and recoil, accommodating changes in fluid volume while maintaining a protective barrier against urine’s toxic components.
Key features and functions include:
- Elasticity: With cuboidal basal cells, polygonal middle layers, and large, oval surface cells, transitional epithelium stretches as the bladder fills, reducing the number of cell layers without compromising integrity.
- Protection: Its tight junctions and thick surface cells prevent urine leakage and protect underlying tissues from chemical damage.
- Regeneration: The tissue’s basal layer undergoes mitosis to replace worn cells, ensuring durability despite constant stretching.
For example, when the bladder is empty, transitional epithelium appears thick with multiple layers, but as it fills, it thins to two or three layers, maintaining a leak-proof barrier. This adaptability is critical for urinary system function, and damage to transitional epithelium, as in urinary tract infections, can lead to inflammation and impaired bladder control.
FAQ 17: What is the role of glandular epithelium in secretion?
Glandular epithelium, a type of specialized epithelial tissue, is composed of cells adapted for secretion, producing substances like mucus, hormones, or enzymes essential for bodily functions. It is found in glands throughout the body and is classified into unicellular and multicellular types based on its structure.
Unicellular glandular epithelium consists of single secretory cells, such as goblet cells in the intestines and respiratory tract, which secrete mucus to lubricate and protect surfaces. Multicellular glandular epithelium forms complex glands, like salivary glands or sweat glands, producing saliva, sweat, or digestive enzymes. These glands may be exocrine (releasing products via ducts) or endocrine (secreting hormones into the bloodstream). The secretory process is regulated by cellular mechanisms, ensuring precise release of substances.
For instance, goblet cells in the stomach secrete mucus to shield the lining from acidic gastric juices, while the pancreas’ glandular epithelium releases digestive enzymes into the small intestine. This secretory role is vital for digestion, thermoregulation, and hormonal balance, making glandular epithelium indispensable.
FAQ 18: How does epithelial tissue contribute to sensory functions?
Sensory epithelium, a type of specialized epithelial tissue, contains neurosensory cells that detect environmental stimuli, such as light, smell, or taste, and transmit signals to the nervous system. Found in sensory organs like the retina, olfactory region, and taste buds, this tissue bridges the external environment and the brain, enabling perception.
Key sensory roles include:
- Light Detection: In the retina, sensory epithelium with photoreceptor cells detects light, initiating visual processing.
- Olfaction: The olfactory epithelium in the nasal cavity contains neurosensory cells that detect odor molecules, enabling smell.
- Taste Perception: Taste buds on the tongue house sensory epithelial cells that identify chemical flavors, contributing to taste.
- Environmental Monitoring: Sensory epithelium in some areas, like the skin, detects touch or temperature changes.
For example, damage to the olfactory epithelium from viral infections can cause loss of smell, as seen in some COVID-19 cases. The integration of sensory epithelium with neural pathways ensures rapid and accurate sensory processing, highlighting its critical role in interaction with the environment.
FAQ 19: Why is epithelial tissue prone to cancer, and what are carcinomas?
Epithelial tissue is susceptible to cancer due to its high regenerative capacity and exposure to environmental stressors like UV radiation, chemicals, or pathogens. Rapid cell division in epithelial layers, such as in the skin or intestines, increases the risk of DNA mutations, which can lead to uncontrolled cell growth. Carcinomas, cancers originating from epithelial tissue, account for approximately 80–90% of human cancers.
Carcinomas develop when epithelial cells undergo malignant transformation, often due to factors like smoking (lung carcinoma), UV exposure (squamous cell carcinoma of the skin), or chronic inflammation (adenocarcinoma in glands). The epithelial-mesenchymal transition (EMT) can exacerbate cancer progression by enabling epithelial tumor cells to become invasive and metastasize. For example, basal cell carcinoma arises from the basal layer of the epidermis, while adenocarcinoma affects glandular tissues like the breast or prostate.
The prevalence of carcinomas underscores the importance of epithelial tissue in cancer research. Early detection through screenings, like colonoscopies for colorectal carcinoma, and targeted therapies are critical for managing these diseases, emphasizing the tissue’s role in health and pathology.
FAQ 20: How is epithelial tissue used in medical and biotechnological advancements?
Epithelial tissue is a focal point in medical and biotechnological research due to its regenerative properties, structural versatility, and role in diseases like cancer. Advances in tissue engineering, regenerative medicine, and drug development leverage epithelial tissue’s characteristics to develop innovative treatments and study physiological processes.
Key applications include:
- Tissue Engineering: Epithelial cells are used to create artificial tissues for transplants, such as lab-grown skin for burn victims, utilizing the epidermis’ regenerative capacity.
- Organoids: Epithelial stem cells are cultured to form organoids, miniature organ-like structures, to study diseases like cystic fibrosis or test drugs, as seen with intestinal organoids.
- Cancer Research: Studying epithelial-derived carcinomas helps develop targeted therapies, such as immunotherapies for squamous cell carcinoma.
- Immune Studies: Intraepithelial lymphocytes in epithelial layers, particularly in the gut, are investigated for their role in immune defense, informing treatments for autoimmune diseases.
- Wound Healing: Research into epithelial regeneration, as in the cornea, guides therapies to accelerate repair.
For example, corneal epithelial stem cell transplants restore vision in patients with damaged corneas, while lung organoids model respiratory diseases like COVID-19. These advancements highlight epithelial tissue’s transformative potential in improving human health and advancing scientific understanding.
Acknowledgement
The development of the article “Epithelial Tissue: The Body’s Protective and Functional Shield” was made possible through the comprehensive information provided by various reputable online sources. These resources offered valuable insights into the structure, function, and significance of epithelial tissue, ensuring the article’s accuracy and depth. The Examsmeta.com website expresses its gratitude to the following websites for their contributions to this work:
- National Institutes of Health: For detailed scientific explanations of epithelial tissue’s role in health and disease.
- PubMed: For access to peer-reviewed studies on epithelial cell biology and pathology.
- Nature: For cutting-edge research on epithelial tissue in regenerative medicine and cancer.
- ScienceDirect: For in-depth articles on epithelial tissue structure and intercellular junctions.
- Khan Academy: For educational content on tissue types and their functions.
- Britannica: For clear and concise descriptions of epithelial tissue characteristics.
- MedlinePlus: For accessible information on epithelial tissue’s role in human anatomy.
- Cleveland Clinic: For insights into epithelial tissue’s clinical relevance in disease and healing.
- Mayo Clinic: For practical explanations of epithelial tissue in medical contexts.
- WebMD: For user-friendly content on epithelial tissue functions and health implications.
- University of Leeds: For academic resources on epithelial tissue histology.
- OpenStax: For open-access educational materials on tissue biology.
- Biology Online: For detailed definitions and classifications of epithelial tissue.
- Histology Guide: For visual and textual resources on epithelial tissue microscopy.
- American Association for Anatomy: For professional insights into epithelial tissue’s anatomical significance.

