Endocrine signaling stands as one of the body’s most fascinating and essential communication networks, allowing distant cells to coordinate complex functions through the release of hormones. These chemical messengers, produced by specialized glands, travel via the bloodstream to influence everything from growth and metabolism to mood and reproduction. In a world where our bodies constantly adapt to internal and external changes, endocrine signaling ensures balance and responsiveness, preventing chaos in physiological processes.
This article dives deep into the intricacies of endocrine signaling, drawing from foundational concepts and expanded insights to provide a comprehensive view. We’ll explore its mechanisms, characteristics, receptors, importance, examples, and much more, including comparisons with other signaling types, evolutionary aspects, and common disorders. Whether you’re a student, health enthusiast, or simply curious about how your body works, this guide breaks it down in straightforward terms.
Table of Contents
What is Signaling in the Body?
Signaling refers to the way cells talk to each other, exchanging information to trigger responses that keep the body functioning smoothly. Imagine cells as tiny workers in a vast factory; they need constant updates to adjust their activities, whether it’s ramping up energy production or defending against invaders. Signaling molecules, often hormones, ions, or proteins, act as these updates, traveling from sender cells to receivers. This process is vital for maintaining homeostasis, the body’s internal equilibrium, and it underpins immune responses, nerve transmissions, and even how we sense the world around us. Without effective signaling, cells would operate in isolation, leading to disarray in critical systems like digestion or heartbeat regulation.
Signaling isn’t just a one-way street; it involves intricate pathways where signals can amplify, dampen, or redirect actions within cells. For instance, when you eat a meal, signaling cues prompt the release of digestive enzymes and adjust blood sugar levels. These pathways often involve cascades of reactions, where one molecule activates another, creating a domino effect that ensures precise control. In broader terms, signaling helps the body respond to stressors, such as exercise or infection, by coordinating multiple organs. It’s a dynamic system, constantly fine-tuned by feedback loops to avoid overreactions or underperformance.
Types of Signaling
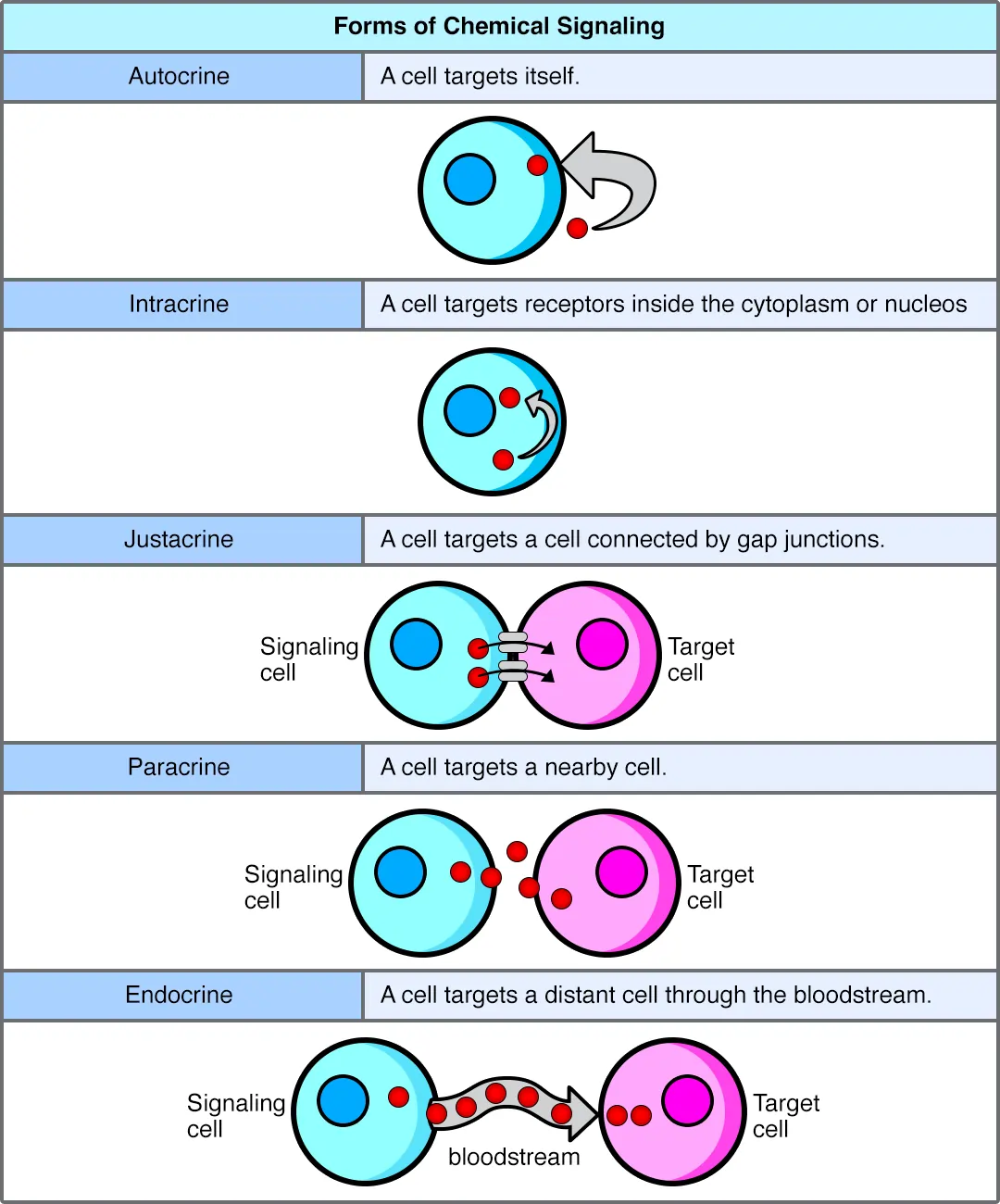
The body employs several signaling strategies, categorized mainly by the distance the signal travels and the target it affects. While some sources stick to three primary types, others include a fourth for specialized neural communication. Each type serves unique purposes, allowing for flexible responses in different scenarios.
- Autocrine Signaling: Here, a cell produces a signal that binds to receptors on its own surface, essentially talking to itself. This self-regulation is common in processes like cell growth and differentiation, where cells need to monitor their own state without external input. For example, cancer cells often exploit autocrine signaling to proliferate uncontrollably.
- Paracrine Signaling: Signals in this category affect nearby cells, creating localized effects. It’s like a neighborhood bulletin where messages spread quickly but don’t go far. This type is crucial in inflammation, where immune cells release factors to recruit help from adjacent tissues, or in development, guiding tissue formation.
- Endocrine Signaling: This involves long-distance communication, with hormones released into the blood to reach distant targets. It’s the focus of our discussion and excels in systemic regulation, such as controlling overall metabolism or growth.
- Neurocrine Signaling: Less common and specific to neurons, this occurs when neurotransmitters bridge gaps between nerve cells. It’s rapid and precise, underpinning quick reflexes and thoughts, though it overlaps with endocrine functions in some hormone-releasing neurons.
These categories aren’t rigid; overlaps exist, like in neuroendocrine signaling where nerves trigger hormone release. Understanding them highlights how the body layers communication for efficiency.
What is Endocrine Signaling?
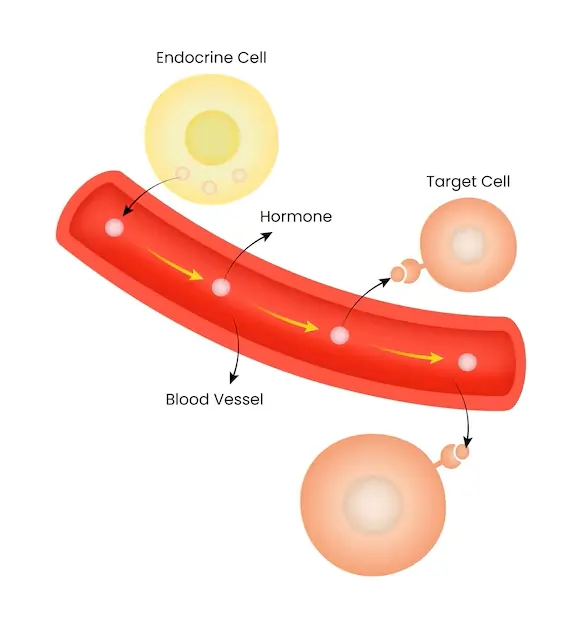
Endocrine signaling represents the body’s long-range messaging system, where endocrine glands secrete hormones that journey through the bloodstream to influence far-off cells. Unlike quicker nerve impulses, this method allows for widespread, sustained effects, making it ideal for ongoing processes like development or stress adaptation. The “endocrine” term derives from Greek roots meaning “secrete within,” reflecting how hormones are dispatched internally rather than externally.
This signaling ties directly to the endocrine system, a network of glands that produce these messengers in response to stimuli like blood chemistry changes or neural inputs. Once released, hormones act as keys, unlocking specific responses in target cells equipped with matching receptors. This specificity prevents random activations, ensuring hormones like insulin affect only glucose-regulating cells. Endocrine signaling’s role extends beyond basics; it integrates with other systems, such as the nervous system, for holistic control.
Key Characteristics of Endocrine Signaling
Endocrine signaling boasts several defining traits that set it apart and enable its effectiveness.
- Hormone Secretion: Glands like the thyroid or pancreas release hormones directly into the blood, bypassing ducts for broad distribution.
- Systemic Effects: By circulating body-wide, hormones can influence multiple organs simultaneously, coordinating responses like energy mobilization during exercise.
- Slow Onset but Prolonged Duration: Unlike instant nerve signals, endocrine effects build gradually but persist, allowing for long-term adjustments in metabolism or growth.
- High Specificity: Each hormone targets cells with complementary receptors, ensuring precise actions without widespread disruption.
- Tight Regulation via Feedback: Negative feedback loops, where rising hormone levels signal glands to reduce production, maintain balance, while positive feedback amplifies responses in scenarios like childbirth.
- Coordination of Processes: It synchronizes bodily functions, from sleep-wake cycles to immune modulation, promoting overall harmony.
These features make endocrine signaling indispensable for adapting to life’s demands, from daily routines to emergencies.
Types of Receptors in Endocrine Signaling
Receptors are the gatekeepers in endocrine signaling, determining which hormones can enter or influence a cell. With countless chemicals circulating, receptors ensure only appropriate ones trigger responses, preventing harmful mix-ups. They fall into two main categories based on location and function.
Surface Receptors: Positioned on the cell membrane, these bind water-soluble hormones like peptides or amines that can’t cross the lipid barrier. Binding activates internal messengers, such as second messengers like cAMP, to relay the signal inward. This is common for quick-acting hormones like adrenaline.
Intracellular Receptors: Located inside the cell, often in the cytoplasm or nucleus, these interact with lipid-soluble hormones like steroids that diffuse through the membrane. Once bound, the complex moves to the DNA, altering gene expression for longer-lasting effects, such as those from cortisol or estrogen.
Receptor diversity allows for nuanced control; some cells have multiple types, enabling layered responses to hormonal cues.
The Mechanism of Endocrine Signaling
Endocrine signaling unfolds in a precise sequence, ensuring signals translate into meaningful actions.
First, hormone secretion occurs when glands respond to triggers, like low blood sugar prompting the pancreas to release glucagon.
Next, circulation carries hormones via blood to distant sites, with transport proteins sometimes aiding solubility or prolonging activity.
Then, receptor recognition happens as hormones dock with specific receptors, fitting like puzzle pieces.
This leads to signal transduction, a relay of intracellular events amplifying the message, often involving enzymes or ion channels.
The result is a cellular response, such as increased protein synthesis or metabolic shifts.
Finally, feedback regulation adjusts output; for example, high thyroid hormone levels inhibit further release from the pituitary.
This mechanism’s elegance lies in its adaptability, allowing fine-tuning based on needs.
Importance of Endocrine Signaling
Endocrine signaling’s impact on health can’t be overstated; it’s the conductor orchestrating bodily harmony.
It regulates growth and development, with hormones like growth hormone shaping bones and muscles from childhood through adulthood.
In metabolic balance, it governs nutrient use, as insulin and glucagon manage glucose for energy stability.
For reproductive function, it oversees cycles, fertility, and pregnancy, with FSH and LH playing starring roles.
During stress responses, cortisol and adrenaline prepare the body for challenges, boosting alertness and resources.
It influences mood and emotions via neurotransmitters modulated by hormones like serotonin.
Moreover, it coordinates environmental adaptations, adjusting to temperature or altitude changes to preserve homeostasis.
Beyond these, it supports immune function, bone health, and even sleep, underscoring its centrality to well-being.
Real-World Examples of Endocrine Signaling
To grasp endocrine signaling, consider these practical illustrations.
Blood Sugar Regulation: The pancreas releases insulin to lower glucose by promoting uptake in cells, while glucagon raises it by liberating stored sugar from the liver.
Calcium Homeostasis: Parathyroid hormone increases blood calcium by drawing from bones and enhancing gut absorption.
Growth Control: Pituitary-derived growth hormone stimulates tissue expansion, affecting height and repair.
Reproductive Cycles: In females, estrogen and progesterone from ovaries regulate menstruation and prepare for pregnancy.
Stress Management: Adrenal glands produce cortisol to suppress non-essential functions and heighten focus during threats.
Thyroid Regulation: TSH prompts thyroid hormone release, influencing metabolism and energy.
These examples show how endocrine signaling maintains daily equilibrium.
Major Endocrine Glands and Their Hormones
The endocrine system comprises several glands, each specializing in certain hormones. Here’s a detailed overview in table form for clarity.
| Gland | Location | Key Hormones | Primary Functions | Common Disorders |
|---|---|---|---|---|
| Hypothalamus | Base of brain | Releasing and inhibiting hormones (e.g., CRH, TRH) | Regulates pituitary, controls appetite, temperature | Hypothalamic dysfunction leading to obesity or temperature dysregulation |
| Pituitary (Master Gland) | Base of brain | GH, TSH, ACTH, FSH, LH, Prolactin, Oxytocin, ADH | Growth, thyroid stimulation, stress response, reproduction, milk production, social bonding, water balance | Pituitary tumors causing acromegaly or Cushing’s disease |
| Thyroid | Neck | Thyroxine (T4), Triiodothyronine (T3), Calcitonin | Metabolism, energy, calcium regulation | Hypothyroidism (fatigue, weight gain), Hyperthyroidism (weight loss, anxiety) |
| Parathyroid | Behind thyroid | Parathyroid hormone (PTH) | Calcium and phosphate balance | Hyperparathyroidism (high calcium, bone weakening) |
| Adrenal | Top of kidneys | Cortisol, Aldosterone, Adrenaline, Noradrenaline | Stress response, electrolyte balance, fight-or-flight | Addison’s disease (low cortisol), Conn’s syndrome (high aldosterone) |
| Pancreas | Abdomen | Insulin, Glucagon, Somatostatin | Blood sugar control, digestion inhibition | Diabetes mellitus (type 1 or 2), Hypoglycemia |
| Gonads (Ovaries/Testes) | Pelvis/Scrotum | Estrogen, Progesterone, Testosterone | Reproduction, secondary sex characteristics | Polycystic ovary syndrome, Hypogonadism |
| Pineal | Brain | Melatonin | Sleep-wake cycles, circadian rhythms | Sleep disorders, seasonal affective disorder |
This table highlights the interconnectedness; for instance, the hypothalamus directs the pituitary, which in turn influences other glands.
Disorders Arising from Endocrine Signaling Issues
When endocrine signaling falters, disorders emerge, often from over or underproduction of hormones. These can stem from gland damage, autoimmune attacks, or genetic factors.
Diabetes, for example, disrupts insulin signaling, leading to high blood sugar and complications like nerve damage. Hypothyroidism slows metabolism due to low thyroid hormones, causing fatigue and cold intolerance. Hyperthyroidism speeds things up, resulting in tremors and heat sensitivity.
Adrenal disorders like Cushing’s syndrome involve excess cortisol, promoting weight gain and high blood pressure, while Addison’s features deficiency, causing weakness and low pressure. Reproductive issues, such as infertility from imbalanced FSH/LH, affect millions.
Treatment often involves hormone replacement, surgery, or medications to restore balance, emphasizing the need for early detection through symptoms like unexplained weight changes or mood swings.
Comparing Endocrine Signaling with Paracrine and Autocrine
To appreciate endocrine signaling’s uniqueness, compare it to its counterparts. The following table outlines key differences.
| Aspect | Autocrine Signaling | Paracrine Signaling | Endocrine Signaling |
|---|---|---|---|
| Distance | Self (same cell) | Short (nearby cells) | Long (distant via blood) |
| Speed | Rapid | Fast, localized | Slower onset, prolonged |
| Examples | Tumor cells stimulating own growth | Wound healing factors attracting immune cells | Insulin regulating body-wide glucose |
| Medium | Direct or local diffusion | Diffusion in extracellular fluid | Bloodstream |
| Regulation | Often self-limited | Feedback from local environment | Systemic feedback loops |
| Role in Body | Cell autonomy, like in immune activation | Tissue repair, inflammation | Overall homeostasis, growth |
This comparison reveals how endocrine excels in global coordination, while others handle immediate, local needs.
The Evolution of Endocrine Signaling in Animals
Endocrine signaling didn’t appear overnight; it evolved over millions of years, starting in simple organisms and becoming sophisticated in vertebrates. In invertebrates like insects, basic hormone-like molecules regulated molting and reproduction, using diffusion rather than blood. As animals developed circulatory systems, endocrine signaling adapted, allowing distant communication.
In early vertebrates, glands like the pituitary emerged, integrating neural and hormonal controls. This hypothalamic-pituitary axis, conserved across species, highlights evolutionary continuity. Hormones such as steroids trace back to ancient pathways, with modifications for new functions like stress responses in land animals.
Environmental pressures drove this evolution; for instance, integrating endocrine with respiratory systems in arthropods helped sense and respond to surroundings. In humans, this legacy means our systems echo those of distant ancestors, aiding research into conserved mechanisms for treating disorders.
Advanced Insights: Feedback Mechanisms in Detail
Feedback is the backbone of endocrine regulation, preventing extremes. Negative feedback, the most common, acts like a thermostat: rising levels inhibit further production. For thyroid function, high T3/T4 suppresses TSH release.
Positive feedback, rarer, escalates responses, as in oxytocin during labor, where contractions trigger more release until delivery.
These loops involve multiple glands; the adrenal axis, for example, starts with hypothalamic CRH prompting pituitary ACTH, which stimulates cortisol, feeding back to dampen the cycle.
Disruptions here cause issues like feedback failure in tumors, leading to unchecked hormone surges.
Hormone Classes and Their Signaling Pathways
Hormones vary by structure, affecting how they signal.
- Peptide Hormones: Short chains like insulin; use surface receptors and second messengers for quick effects.
- Steroid Hormones: Lipid-based like cortisol; intracellular receptors alter genes for sustained changes.
- Amine Hormones: Derived from amino acids, like thyroid hormones (intracellular) or catecholamines (surface).
This diversity allows tailored responses, from seconds to days.
Everyday Impacts and Lifestyle Tips
Endocrine signaling influences daily life profoundly. Poor diet can disrupt insulin signaling, leading to metabolic syndrome. Exercise boosts endorphins and growth factors, enhancing mood and muscle repair.
To support it, maintain balanced nutrition, manage stress through mindfulness, and get adequate sleep, as melatonin relies on circadian cues. Regular check-ups catch imbalances early.
In medicine, understanding this aids therapies like hormone replacement for menopause or insulin pumps for diabetes.
Conclusion
Endocrine signaling orchestrates the body’s intricate dance, from subtle metabolic tweaks to dramatic stress responses. By secreting hormones that traverse the bloodstream to precise targets, it ensures cohesion amid constant change. We’ve explored its mechanisms, receptors, importance, examples, glands, disorders, comparisons, and evolutionary roots, revealing a system both ancient and adaptable. As research advances, insights into this network promise better health outcomes, reminding us of the body’s remarkable resilience. Appreciating endocrine signaling deepens our awe for the human form, encouraging proactive care for this vital communicator.
Frequently Asked Questions
FAQ 1: What is the primary function of endocrine signaling in the body?
Endocrine signaling serves as the body’s long-distance communication tool, using hormones to coordinate a wide array of functions that keep everything running smoothly. At its heart, this process involves specialized glands releasing chemical messengers into the bloodstream, which then travel to distant cells to trigger specific responses. This isn’t just about quick fixes; it’s about maintaining overall balance, or what scientists call homeostasis, ensuring that things like body temperature, energy levels, and even emotional states stay stable despite constant changes in our environment or daily activities.
Think about how this plays out in real terms. When you’re under stress, endocrine signaling kicks in to release hormones like cortisol, which help mobilize energy reserves and sharpen your focus. Over time, this system influences bigger picture elements, such as growth during childhood or reproductive cycles in adulthood. Without it, the body would struggle to adapt, leading to imbalances that could affect everything from sleep patterns to immune responses. Researchers have noted that endocrine signaling is crucial for processes like nutrient breakdown and storage, highlighting its role in preventing metabolic disorders.
Moreover, this signaling pathway integrates with other bodily systems to ensure seamless operation. For instance, it works hand in hand with the digestive system to regulate appetite and with the skeletal system to maintain bone density. Studies emphasize that disruptions in endocrine signaling can lead to widespread issues, underscoring its foundational importance in health. In essence, endocrine signaling isn’t a background player; it’s the conductor that harmonizes the body’s complex symphony, allowing us to thrive in a dynamic world.
FAQ 2: How do feedback loops regulate endocrine signaling?
Feedback loops are essential mechanisms that fine-tune hormone levels in endocrine signaling, acting much like a thermostat to prevent extremes and maintain stability. These loops monitor hormone concentrations and adjust production accordingly, ensuring the body responds appropriately without overdoing it. In most cases, they operate on a principle of checks and balances, where the output of a process influences its own input.
- Negative Feedback Loops: This is the most common type, where rising hormone levels signal the gland to slow down or stop production. For example, when thyroid hormones reach optimal levels in the blood, they inhibit the release of thyroid-stimulating hormone from the pituitary gland, preventing overactivity and maintaining metabolic equilibrium. This self-stabilizing approach is vital for homeostasis, as it counters changes and restores balance, much like how insulin lowers blood sugar after a meal and then tapers off as levels normalize.
- Positive Feedback Loops: Less frequent but powerful, these amplify a response by encouraging more hormone release. A classic case is during childbirth, where oxytocin stimulates contractions, which in turn prompt more oxytocin, escalating until delivery occurs. While effective for short bursts, positive loops are tightly controlled to avoid runaway effects.
- Short-Loop and Long-Loop Feedback: In short-loop systems, pituitary hormones directly influence the hypothalamus to adjust its signals, providing quick corrections. Long-loop feedback involves hormones from peripheral glands feeding back to both the pituitary and hypothalamus for broader regulation, as seen in the adrenal system’s control of cortisol. These layered controls highlight how feedback loops not only regulate but also integrate endocrine signaling with the body’s needs.
Overall, these loops ensure efficiency, with disruptions potentially leading to conditions like hormone imbalances. By constantly adapting, they support everything from daily energy management to long-term health.
FAQ 3: What are the major endocrine glands and the hormones they produce?
The endocrine system features several key glands that produce hormones essential for regulating bodily functions. Below is a detailed table outlining these glands, their locations, primary hormones, main functions, and associated common issues, drawing from established physiological knowledge.
| Gland | Location | Primary Hormones | Main Functions | Common Associated Issues |
|---|---|---|---|---|
| Hypothalamus | Base of the brain | Corticotropin-releasing hormone (CRH), Thyrotropin-releasing hormone (TRH), Gonadotropin-releasing hormone (GnRH) | Acts as a control center, regulating the pituitary gland and influencing appetite, temperature, and stress responses | Dysfunction can lead to issues like irregular body temperature or appetite disorders, often linked to stress or injury |
| Pituitary Gland (often called the master gland) | Base of the brain, attached to the hypothalamus | Growth hormone (GH), Thyroid-stimulating hormone (TSH), Adrenocorticotropic hormone (ACTH), Follicle-stimulating hormone (FSH), Luteinizing hormone (LH), Prolactin, Oxytocin, Antidiuretic hormone (ADH) | Controls growth, metabolism, stress responses, reproduction, milk production, social bonding, and water balance | Tumors or deficiencies may cause conditions such as acromegaly (excess GH) or hypopituitarism, affecting multiple systems |
| Thyroid Gland | Front of the neck | Thyroxine (T4), Triiodothyronine (T3), Calcitonin | Regulates metabolism, energy production, heart rate, and calcium levels in the blood | Hypothyroidism (low hormone levels leading to fatigue and weight gain) or hyperthyroidism (excess causing anxiety and weight loss) |
| Parathyroid Glands | Behind the thyroid gland | Parathyroid hormone (PTH) | Maintains calcium and phosphate balance, supporting bone health and nerve function | Hyperparathyroidism can result in high blood calcium, weakening bones and causing kidney stones |
| Adrenal Glands | On top of each kidney | Cortisol, Aldosterone, Adrenaline (epinephrine), Noradrenaline (norepinephrine) | Manages stress responses, electrolyte balance, blood pressure, and the fight-or-flight reaction | Addison’s disease (insufficient cortisol leading to fatigue) or Cushing’s syndrome (excess cortisol causing weight gain and high blood pressure) |
| Pancreas | Behind the stomach in the abdomen | Insulin, Glucagon, Somatostatin | Controls blood sugar levels, aids digestion, and inhibits excessive hormone release | Diabetes (type 1 or 2, from insulin issues) or hypoglycemia (low blood sugar episodes) |
| Gonads (Ovaries in females, Testes in males) | Pelvis (ovaries) or scrotum (testes) | Estrogen, Progesterone (ovaries); Testosterone (testes) | Oversees reproductive development, menstrual cycles, sperm production, and secondary sex characteristics | Conditions like polycystic ovary syndrome or low testosterone levels affecting fertility and mood |
| Pineal Gland | Center of the brain | Melatonin | Regulates sleep-wake cycles and circadian rhythms | Disruptions can lead to sleep disorders or seasonal affective disorder, often influenced by light exposure |
This table illustrates the interconnected nature of these glands, where one often influences another to maintain bodily harmony.
FAQ 4: Can you explain how hormones travel through the bloodstream to their target cells?
Hormones begin their journey when secreted by endocrine glands directly into the bloodstream, a process that allows them to circulate throughout the body efficiently. Unlike other substances that might be filtered out quickly, hormones are designed to linger just long enough to reach their destinations. Some, like steroid hormones, are lipid-soluble and can diffuse easily across cell membranes, while others, such as peptide hormones, are water-soluble and rely on binding to surface receptors to initiate their effects. This selective travel ensures that only cells with the right receptors respond, preventing unnecessary activations elsewhere.
As they move through the blood, hormones often hitch a ride on carrier proteins, which protect them from degradation and help regulate their availability. For instance, thyroid hormones bind to proteins like thyroxine-binding globulin, extending their half-life and allowing controlled release to tissues. This binding also modulates how quickly hormones act, with free-floating ones available for immediate use and bound ones serving as a reserve. Factors like blood flow and organ perfusion influence delivery speed, meaning active areas like muscles during exercise might receive more hormones faster.
Upon arrival at target cells, hormones lock onto specific receptors, triggering a cascade of internal changes. This could mean altering gene expression for long-term effects or activating enzymes for quicker responses. The entire process highlights the precision of endocrine signaling, where travel isn’t random but a targeted delivery system. Disruptions, such as in transport proteins, can lead to imbalances, emphasizing the need for healthy circulation. Overall, this bloodstream voyage underscores how hormones act as vital messengers, bridging distant parts of the body for coordinated function.
FAQ 5: What role does endocrine signaling play in regulating metabolism?
Endocrine signaling is a cornerstone in managing metabolism, the process by which the body converts food into energy and building blocks for growth. Hormones act as regulators, adjusting metabolic rates to match the body’s needs, whether it’s ramping up during activity or conserving during rest. For example, thyroid hormones like T3 and T4 set the baseline metabolic rate, influencing how quickly cells burn calories and produce heat. Without proper endocrine input, metabolism could slow to a crawl or accelerate uncontrollably, leading to fatigue or unintended weight changes.
This regulation extends to nutrient handling, where insulin from the pancreas signals cells to absorb glucose for energy or storage, preventing spikes in blood sugar after meals. Conversely, glucagon steps in during fasting to release stored glucose, maintaining steady energy supply. Adrenal hormones like cortisol also play a part, especially under stress, by promoting the breakdown of fats and proteins for quick fuel. Research shows that endocrine disruptions, such as in diabetes, can derail these processes, highlighting the system’s sensitivity to lifestyle factors like diet and exercise.
Beyond basics, endocrine signaling coordinates with other systems for holistic metabolic control. It influences appetite through hormones like leptin from fat tissues, which signals fullness to the brain, and ghrelin from the stomach, which prompts hunger. In aging or disease, these signals can weaken, affecting energy balance. Advances in understanding this role have led to therapies targeting metabolic pathways, underscoring endocrine signaling’s profound impact on daily vitality and long-term health.
FAQ 6: How does the endocrine system interact with the nervous system?
The endocrine and nervous systems collaborate closely, forming a dynamic partnership that blends rapid electrical signals with slower, sustained hormonal responses to manage body functions. This interaction, often termed neuroendocrine integration, allows for comprehensive control over behaviors, emotions, and physiological adjustments. The hypothalamus serves as a key bridge, receiving neural inputs and translating them into hormonal directives via the pituitary gland.
- Shared Regulation of Stress: When the nervous system detects a threat, it activates the sympathetic branch, prompting the adrenal glands to release adrenaline for immediate fight-or-flight actions. Endocrine signaling follows with cortisol to sustain the response, modulating energy and immune function over time.
- Influence on Behavior and Mood: Hormones like oxytocin, released during social interactions detected by the nervous system, enhance bonding and trust. Conversely, neural activity in the brain can alter hormone production, as seen in how chronic stress affects thyroid function.
- Homeostasis Maintenance: The nervous system monitors internal conditions via sensors and signals the endocrine system to adjust, such as in temperature regulation where neural cues prompt sweat gland activation alongside hormonal shifts in metabolism.
- Reproductive Coordination: Neural signals from the brain trigger gonadotropin-releasing hormone, leading to pituitary hormones that drive reproductive cycles, illustrating bidirectional communication.
This interplay ensures adaptability, with disruptions potentially causing issues like anxiety or hormonal imbalances. By working together, these systems provide layered responses, from instant reflexes to enduring adaptations.
FAQ 7: What are some common endocrine disorders and their treatments?
Endocrine disorders arise from imbalances in hormone production or signaling, affecting millions worldwide. The table below details several prevalent conditions, their causes, symptoms, and standard treatments, based on clinical insights.
| Disorder | Common Causes | Key Symptoms | Standard Treatments | Potential Complications if Untreated |
|---|---|---|---|---|
| Diabetes Mellitus (Type 1 and Type 2) | Autoimmune destruction of insulin-producing cells (Type 1); Insulin resistance often due to lifestyle factors (Type 2) | Frequent urination, excessive thirst, unexplained weight loss, fatigue | Insulin injections or pumps for Type 1; Oral medications, diet changes, and exercise for Type 2; Monitoring blood sugar levels | Nerve damage, kidney failure, cardiovascular issues |
| Hypothyroidism | Autoimmune conditions like Hashimoto’s, iodine deficiency, or thyroid surgery | Weight gain, fatigue, cold intolerance, dry skin, depression | Synthetic thyroid hormone replacement like levothyroxine; Regular blood tests to adjust dosage | Heart problems, infertility, severe cases leading to myxedema coma |
| Hyperthyroidism (including Graves’ Disease) | Autoimmune overactivation, nodules, or excess iodine | Weight loss, rapid heartbeat, anxiety, heat intolerance, tremors | Antithyroid drugs like methimazole, radioactive iodine therapy, or surgery to remove part of the thyroid | Heart arrhythmias, bone thinning, eye problems in Graves’ cases |
| Cushing’s Syndrome | Excess cortisol from tumors, prolonged steroid use, or pituitary issues | Weight gain in the face and abdomen, high blood pressure, easy bruising, muscle weakness | Surgery to remove tumors, medications to block cortisol production, or gradual tapering of steroids | Osteoporosis, diabetes, increased infection risk |
| Addison’s Disease | Autoimmune damage to adrenal glands, infections, or genetic factors | Fatigue, weight loss, low blood pressure, skin darkening, salt cravings | Hormone replacement with corticosteroids and mineralocorticoids; Emergency kits for crises | Life-threatening adrenal crisis during stress |
| Polycystic Ovary Syndrome (PCOS) | Genetic and environmental factors leading to hormone imbalances | Irregular periods, excess hair growth, acne, weight gain, infertility | Lifestyle changes, birth control pills for cycle regulation, metformin for insulin resistance | Increased risk of diabetes, heart disease, endometrial cancer |
| Acromegaly | Pituitary tumor causing excess growth hormone | Enlarged hands and feet, facial changes, joint pain, headaches | Surgery to remove the tumor, medications like somatostatin analogs, or radiation therapy | Arthritis, diabetes, cardiovascular complications |
| Hyperparathyroidism | Benign tumors on parathyroid glands, vitamin D deficiency | Fatigue, bone pain, kidney stones, frequent urination | Surgery to remove overactive glands, medications to manage calcium levels | Osteoporosis, kidney damage |
Early diagnosis through blood tests and imaging is key, with treatments often tailored to individual needs for optimal outcomes.
FAQ 8: Provide examples of endocrine signaling in everyday activities.
Endocrine signaling quietly powers many routine aspects of life, from waking up to handling meals. It’s not always noticeable, but its effects shape how we feel and function daily.
- Morning Wake-Up and Energy Boost: As daylight hits, the pineal gland reduces melatonin production, signaling the body to wake. Meanwhile, cortisol from the adrenals peaks, providing an energy surge to start the day, regulated by circadian rhythms.
- Meal Digestion and Blood Sugar Control: After eating, the pancreas releases insulin to help cells absorb glucose, preventing energy crashes. Glucagon counters this if sugar dips, ensuring steady focus during work or school.
- Exercise Response: During a workout, adrenaline ramps up heart rate and frees up glucose for muscles, while growth hormone later aids repair and building strength.
- Stress Management in Traffic: A sudden jam triggers cortisol release, heightening alertness to navigate safely, then tapering off to avoid prolonged tension.
- Sleep Preparation: In the evening, rising melatonin dims activity, promoting restful sleep essential for recovery.
These examples show how endocrine signaling adapts to daily demands, supporting health when balanced.
FAQ 9: What are the differences between positive and negative feedback in endocrine regulation?
Positive and negative feedback mechanisms in endocrine regulation represent two contrasting ways the body controls hormone levels, each suited to different scenarios. Negative feedback, the predominant type, works by counteracting changes to restore equilibrium. When a hormone’s concentration rises too high, it signals upstream glands to reduce production, much like a cooling system kicking in when a room gets too warm. This prevents overaccumulation and maintains steady states, crucial for ongoing processes like blood pressure or temperature control.
In contrast, positive feedback escalates a response, pushing the system further in one direction until a specific goal is achieved. It acts as an amplifier, where initial hormone release triggers more of the same, creating a snowball effect. This is rare in endocrinology because unchecked escalation could be harmful, but it’s perfectly timed for events needing rapid intensification, such as labor contractions driven by oxytocin. Once the event concludes, the loop breaks, avoiding persistence.
The key distinction lies in their outcomes: negative feedback stabilizes, while positive accelerates toward completion. Both are integral, with negative dominating daily homeostasis and positive handling acute needs. Imbalances in these can lead to disorders, like failed negative feedback causing excess hormones. Understanding this duality reveals the endocrine system’s sophisticated design for adaptability.
FAQ 10: How does endocrine signaling contribute to growth and development?
Endocrine signaling is pivotal in guiding growth and development from infancy through adulthood, orchestrating changes that shape our physical and functional maturity. Starting in the womb, hormones like those from the placenta set the stage for organ formation and fetal growth. Post-birth, the pituitary gland’s growth hormone takes center stage, stimulating bone elongation and muscle building during childhood spurts. This hormone works synergistically with others, such as thyroid hormones, which ensure proper metabolic support for these energy-intensive processes.
As puberty hits, endocrine shifts become more pronounced, with gonadotropins from the pituitary prompting the gonads to produce sex hormones like estrogen and testosterone. These drive secondary characteristics, from voice deepening to breast development, while also influencing bone density and height finalization. Beyond physicality, endocrine signaling affects cognitive and emotional growth, with hormones modulating brain development and mood stability. Deficiencies here can stunt progress, while excesses might cause premature changes.
Into adulthood, the system transitions to maintenance, with hormones like insulin-like growth factors aiding tissue repair and preventing degeneration. Aging brings gradual declines, but healthy signaling can mitigate issues like osteoporosis. Research links optimal endocrine function to longevity, emphasizing nutrition and activity’s role in supporting it. Ultimately, endocrine signaling’s contributions weave a lifelong narrative of transformation and resilience.
FAQ 11: How has endocrine signaling evolved in animals?
The evolution of endocrine signaling in animals reveals a fascinating journey from simple chemical messengers in ancient organisms to the sophisticated hormonal networks we see today. Starting with early invertebrates, basic signaling molecules helped coordinate essential functions like reproduction and molting, relying on diffusion rather than a circulatory system. As animals developed more complex bodies, endocrine signaling adapted, incorporating blood-like fluids to carry hormones over longer distances. This shift allowed for better integration between organs, enabling responses to environmental changes that were crucial for survival on land or in diverse habitats.
Over time, key innovations emerged, such as the hypothalamic-pituitary axis in vertebrates, which acts as a central command center linking neural and hormonal controls. This structure, conserved across species from fish to humans, underscores evolutionary continuity, where ancient pathways were repurposed for new roles. For instance, steroid hormones, which trace back to primordial signals, evolved to manage stress, metabolism, and reproduction in more advanced animals. Researchers note that environmental pressures drove these changes; in arthropods, endocrine systems integrated with respiratory mechanisms to sense surroundings, while in mammals, they became finely tuned for social behaviors and longevity.
Further insights come from comparative studies, showing how endocrine disruptors mimic ancient signals, highlighting the system’s vulnerability inherited from evolutionary history. In embryos, these signals guide development, echoing patterns seen in fossil records. As species diversified, endocrine signaling interpolated new steps into pathways, adding layers of regulation for precision. This progression not only enhanced adaptability but also set the stage for human health issues when disrupted. Understanding this evolution aids modern medicine, offering clues to treat disorders by targeting conserved mechanisms.
FAQ 12: What lifestyle factors can influence endocrine health?
Maintaining endocrine health involves mindful choices in daily habits, as various lifestyle elements directly impact hormone production and balance. Diet plays a central role, with nutrient-rich foods supporting gland function, while excessive sugar or processed items can lead to insulin resistance and metabolic strain. Physical activity boosts hormone regulation, enhancing insulin sensitivity and reducing stress-related cortisol spikes, but overexercising might disrupt reproductive hormones.
Stress management is another key area, as chronic tension elevates cortisol, potentially suppressing thyroid and adrenal functions over time. Quality sleep aligns with circadian rhythms, allowing proper melatonin release and hormone recovery, whereas irregular patterns can imbalance growth hormone and appetite regulators like leptin.
- Nutrition Choices: Incorporating omega-3s, vitamins, and minerals from whole foods aids thyroid and adrenal health, while avoiding endocrine disruptors in plastics or pesticides minimizes interference with natural signals.
- Exercise Routines: Moderate aerobic and strength training promotes endorphin release and metabolic harmony, but balance is essential to prevent overtraining syndrome affecting cortisol and testosterone.
- Stress Reduction Techniques: Practices like meditation or yoga lower chronic stress hormones, supporting overall endocrine resilience and preventing issues like adrenal fatigue.
- Sleep Hygiene: Aiming for 7-9 hours nightly optimizes hormonal cycles, with consistent bedtimes enhancing melatonin and growth hormone secretion for repair and mood stability.
- Environmental Exposures: Limiting contact with chemicals in cosmetics or household products reduces disruption to estrogen and thyroid pathways, fostering long-term endocrine well-being.
By integrating these factors, individuals can proactively support their endocrine system, potentially warding off disorders and enhancing vitality.
FAQ 13: How does endocrine signaling differ between plants and animals?
Endocrine signaling showcases intriguing contrasts between plants and animals, reflecting their unique evolutionary paths and physiological needs. The table below outlines key differences, drawing from biological comparisons to highlight how each kingdom adapts signaling for survival.
| Aspect | Plants | Animals |
|---|---|---|
| Primary Messengers | Plant hormones like auxins, cytokinins, and ethylene, which are small molecules regulating growth and responses to light or gravity. | Animal hormones such as insulin, cortisol, and estrogen, produced by specialized glands for systemic control. |
| Transport Mechanism | Diffusion through cell walls or vascular tissues like xylem and phloem; no bloodstream equivalent. | Circulation via the bloodstream, allowing rapid, long-distance delivery to distant targets. |
| Speed and Duration | Often slower, with effects building over days for growth adjustments; sustained for environmental adaptation. | Can be quick for acute responses like adrenaline surges, or prolonged for development. |
| Receptors and Pathways | Mainly enzyme-linked receptors on cell surfaces; signals often involve gene activation for tropisms. | Mix of surface and intracellular receptors; pathways include second messengers for diverse effects. |
| Integration with Other Systems | Closely tied to environmental cues via plasmodesmata for cell-to-cell communication, lacking a nervous system. | Intertwined with the nervous system for neuroendocrine responses, enabling complex behaviors. |
| Examples of Functions | Regulates seed germination, fruit ripening, and defense against herbivores through jasmonic acid. | Manages metabolism, reproduction, and stress via pituitary and adrenal hormones. |
| Evolutionary Notes | Evolved for sessile lifestyle, focusing on local and environmental signaling without mobility. | Adapted for movement and social interactions, emphasizing internal homeostasis. |
These distinctions emphasize how endocrine-like signaling in plants supports stationary life, while in animals, it facilitates dynamic responses.
FAQ 14: What is the role of the endocrine system in the immune response?
The endocrine system plays a pivotal supportive role in the immune response, acting as a modulator that fine-tunes how the body defends against threats. Hormones serve as bridges, influencing immune cell activity and ensuring responses are neither too weak to combat invaders nor overly aggressive, which could lead to autoimmunity. For instance, during infection or injury, cortisol from the adrenals helps dampen inflammation once the initial threat subsides, preventing tissue damage from prolonged immune activation. This hormonal oversight integrates with the nervous system, creating a triad that coordinates stress, immunity, and recovery.
Sex hormones like estrogen and testosterone add another layer, explaining why immune responses can differ between genders. Estrogen often enhances antibody production and innate immunity, potentially offering protection but also raising risks for autoimmune conditions in women. Thyroid hormones further contribute by regulating metabolic support for immune cells, ensuring they have the energy to proliferate and function effectively. Disruptions in this interplay, such as low thyroid levels, can weaken defenses, making infections more severe.
In chronic scenarios, endocrine signals help adapt immunity over time, like during pregnancy where hormones suppress certain responses to protect the fetus. This bidirectional communication means immune cells express hormone receptors, allowing direct influence, while cytokines from immune activity can feedback to adjust hormone release. Overall, the endocrine system’s involvement ensures a balanced, adaptive immune landscape, crucial for health in the face of daily challenges.
FAQ 15: What are some recent advances in endocrinology research as of 2025?
Recent strides in endocrinology have transformed how we approach hormone-related conditions, leveraging technology and deeper insights into biology. As of 2025, focus has shifted toward personalized treatments, with genetic profiling enabling tailored therapies for diabetes and thyroid disorders. Innovations like continuous glucose monitors integrated with AI predict blood sugar fluctuations, improving management for millions.
- Precision Medicine for Diabetes: Advances in beta-cell regeneration and stem cell therapies offer hope for curing type 1 diabetes, with trials showing restored insulin production.
- AI in Hormone Analysis: Machine learning algorithms analyze endocrine data for early detection of imbalances, enhancing diagnostics for PCOS and adrenal issues.
- Incretin-Based Therapies: New drugs mimicking gut hormones like GLP-1 provide dual benefits for obesity and diabetes, with extended-release formulations reducing injection frequency.
- Endocrine Disruptor Research: Studies on environmental chemicals have led to biomarkers for exposure, guiding preventive strategies in public health.
- Neuroendocrine Integration: Breakthroughs in brain-hormone links are advancing treatments for mood disorders tied to endocrine dysfunction, using targeted neuromodulation.
These developments promise more effective, less invasive care, emphasizing prevention and integration with other medical fields.
FAQ 16: What are endocrine disruptors and how do they affect human health?
Endocrine disruptors are chemicals that interfere with hormone systems, posing risks to health. The table below details common types, sources, effects, and mitigation strategies, based on extensive research.
| Disruptor Type | Common Sources | Health Effects | Mitigation Tips | Key Research Insights |
|---|---|---|---|---|
| Bisphenol A (BPA) | Plastics, food cans, receipts | Mimics estrogen, linked to fertility issues, obesity, and developmental delays. | Use BPA-free products, avoid heating plastics. | Studies show early exposure alters brain development. |
| Phthalates | Cosmetics, fragrances, toys | Disrupts testosterone, associated with reproductive problems and metabolic disorders. | Choose phthalate-free personal care items. | Linked to reduced sperm quality in men. |
| PFAS (Forever Chemicals) | Non-stick cookware, waterproof fabrics | Affects thyroid function, increasing cancer and immune risks. | Filter water, opt for natural materials. | Persistent in body, contributing to widespread contamination. |
| Pesticides (e.g., DDT) | Agricultural residues, home sprays | Interferes with multiple hormones, leading to neurological and endocrine cancers. | Eat organic produce, use natural pest control. | Banned in many places but legacy effects persist. |
| Flame Retardants (PBDEs) | Furniture, electronics | Thyroid disruption, impacting cognition and behavior in children. | Ventilate spaces, choose flame-retardant-free items. | Accumulates in breast milk, affecting infants. |
| Dioxins | Industrial pollution, fatty meats | Alters sex hormones, raising risks for diabetes and immune suppression. | Reduce animal fat intake, support clean air policies. | Long-term exposure tied to generational effects. |
Awareness and regulation are key to minimizing these impacts.
FAQ 17: How do hormones influence the aging process?
Hormones profoundly shape the aging process, acting as regulators that decline or shift with time, affecting everything from physical vitality to cognitive sharpness. As we age, levels of growth hormone drop, leading to reduced muscle mass, slower metabolism, and diminished bone density, which can contribute to frailty. This natural ebb influences repair mechanisms, making tissues more susceptible to wear and tear. Estrogen in women and testosterone in men also wane, impacting mood, energy, and cardiovascular health, often manifesting as menopause or andropause symptoms.
Thyroid hormones play a subtle yet critical role, with slight decreases potentially slowing metabolic rates and exacerbating fatigue or weight gain. Insulin sensitivity changes too, heightening risks for diabetes as cells become less responsive. These shifts aren’t just inevitable; lifestyle factors like exercise can mitigate declines, preserving hormone function longer. Research suggests that balanced hormones support longevity by bolstering immune resilience and reducing inflammation.
In the brain, hormones like melatonin regulate sleep, which deteriorates with age, affecting recovery and mental acuity. Interventions such as hormone replacement therapy aim to restore balance, though they’re tailored to avoid risks. Ultimately, hormones orchestrate aging’s pace, offering avenues for healthier later years through informed management.
FAQ 18: How is endocrine signaling linked to mental health disorders?
Endocrine signaling intersects with mental health in profound ways, where hormonal imbalances can precipitate or exacerbate disorders. Thyroid dysfunction, for instance, often mimics depression with low energy and mood dips, while hyperthyroidism might fuel anxiety through rapid heart rates and restlessness.
- Stress Hormones and Anxiety: Elevated cortisol from chronic stress disrupts brain chemistry, heightening anxiety and contributing to PTSD-like symptoms.
- Reproductive Hormones in Mood Swings: Fluctuations in estrogen and progesterone during cycles or menopause can trigger depression or irritability.
- Insulin and Cognitive Health: Poor glucose regulation in diabetes links to cognitive decline and increased Alzheimer’s risk.
- Adrenal Issues in Psychiatric Symptoms: Conditions like Cushing’s syndrome present with psychosis or mania due to excess cortisol.
- Pituitary Disorders: Tumors affecting growth hormone or prolactin may lead to emotional instability or schizophrenia-like features.
Addressing these links through endocrine checks can improve mental health outcomes.
FAQ 19: What are the main differences between endocrine and exocrine glands?
Endocrine and exocrine glands serve distinct roles in secretion. The table below compares them comprehensively.
| Feature | Endocrine Glands | Exocrine Glands |
|---|---|---|
| Secretion Type | Hormones directly into bloodstream. | Enzymes, sweat, or mucus via ducts to surfaces or organs. |
| Duct Presence | Ductless; releases internally. | Ducted; directs to specific sites. |
| Examples | Thyroid, pituitary, adrenals. | Salivary, sweat, pancreatic (exocrine part). |
| Function Scope | Systemic effects on distant targets. | Localized actions like digestion or lubrication. |
| Regulation | Feedback loops with nervous system. | Often neural or local stimuli. |
| Speed of Action | Slower, sustained responses. | Faster, immediate effects. |
| Health Impacts | Imbalances cause widespread disorders like diabetes. | Issues lead to local problems like dry mouth. |
This distinction highlights their complementary contributions to bodily function.
FAQ 20: What future trends are emerging in endocrine medicine and treatments?
The landscape of endocrine medicine is evolving rapidly, with trends pointing toward more personalized and tech-driven approaches. Precision medicine, fueled by genetic insights, allows treatments customized to individual hormone profiles, potentially revolutionizing care for conditions like PCOS or hypothyroidism. AI integration in diagnostics promises faster, more accurate assessments, analyzing vast data sets to predict disease progression and optimize therapies.
Non-invasive delivery methods, such as inhaled insulins or smart patches, are gaining traction, improving compliance and reducing side effects. Stem cell research holds promise for regenerating endocrine tissues, offering cures rather than management for diabetes. Focus on endocrine disruptors is driving preventive strategies, with biomarkers guiding environmental health policies.
Telemedicine and wearable monitors will empower patients, enabling real-time hormone tracking and virtual consultations. As research advances, integrative therapies combining hormones with lifestyle interventions could enhance outcomes, emphasizing holistic well-being in an aging population.
Acknowledgement
The development of the article “Endocrine Signaling: Mechanisms, Types, and Role in Human Health” was made possible through the wealth of information provided by several reputable sources. The Examsmeta.com website expresses its sincere gratitude to National Institute of Diabetes and Digestive and Kidney Diseases (www.niddk.nih.gov), Endocrine Society (www.endocrine.org), Mayo Clinic (www.mayoclinic.org), and PubMed (www.ncbi.nlm.nih.gov/pubmed) for their comprehensive and reliable resources on endocrine signaling, hormonal mechanisms, and related disorders.
These platforms offered invaluable insights into the scientific and clinical aspects of endocrinology, ensuring the article’s accuracy and depth. Their contributions were instrumental in crafting a detailed and accessible exploration of this vital biological process.

