Connective tissue is a fundamental component of the body, serving as the structural scaffolding that supports, binds, and separates various tissues and organs. Its remarkable diversity and functionality make it indispensable to the body’s integrity and homeostasis. From the flexible cartilage in joints to the fluid matrix of blood, connective tissue plays a multifaceted role in providing support, facilitating transport, and enabling immune defense. This article explores the definition, types, functions, examples, and disorders of connective tissue, delving into its intricate composition and critical contributions to bodily functions.
Table of Contents
Understanding Connective Tissue
Connective tissue is one of the four primary tissue types in the body, alongside epithelial, muscle, and nervous tissues. Unlike other tissues, connective tissue is characterized by its extracellular matrix, a complex network of protein fibers and a gel-like ground substance that provides strength, elasticity, and resilience. This matrix is secreted by specialized cells, such as fibroblasts, adipocytes, and immune cells, which are embedded within it. The extracellular matrix varies widely among connective tissue types, allowing them to perform diverse roles, from providing structural support to enabling nutrient transport.
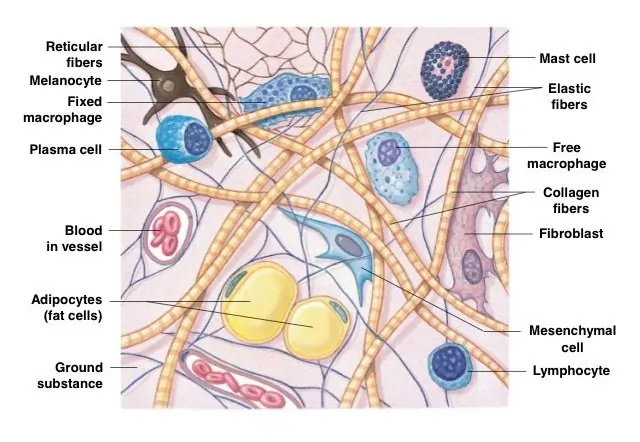
Connective tissues are ubiquitous, found in nearly every part of the body. They connect muscles to bones, bind organs together, and protect delicate structures from mechanical stress. Their versatility stems from the varying proportions of cells, fibers, and ground substance, which give rise to different types, such as loose connective tissue, dense connective tissue, and specialized connective tissue like cartilage, bone, and blood. Beyond structural support, connective tissues contribute to energy storage, insulation, and immune responses, making them essential for survival and overall health.
Types of Connective Tissue
Connective tissue is broadly categorized into three main types: loose connective tissue, dense connective tissue, and specialized connective tissue. Each type is tailored to specific functions, determined by the composition and arrangement of its extracellular matrix and cells. Below, we explore these types in detail, highlighting their structure, locations, and roles in the body.
Loose Connective Tissue
Loose connective tissue is the most widespread type, characterized by a loosely arranged network of collagen and elastin fibers within a gel-like matrix. This tissue provides flexibility, cushioning, and support to organs, blood vessels, and nerves. It is found beneath the skin (subcutaneous layer), around blood vessels, and within mucous membranes. A key subtype is areolar tissue, which serves as a universal packing material, filling spaces between organs and tissues. Another important subtype is adipose tissue, which specializes in fat storage and insulation.
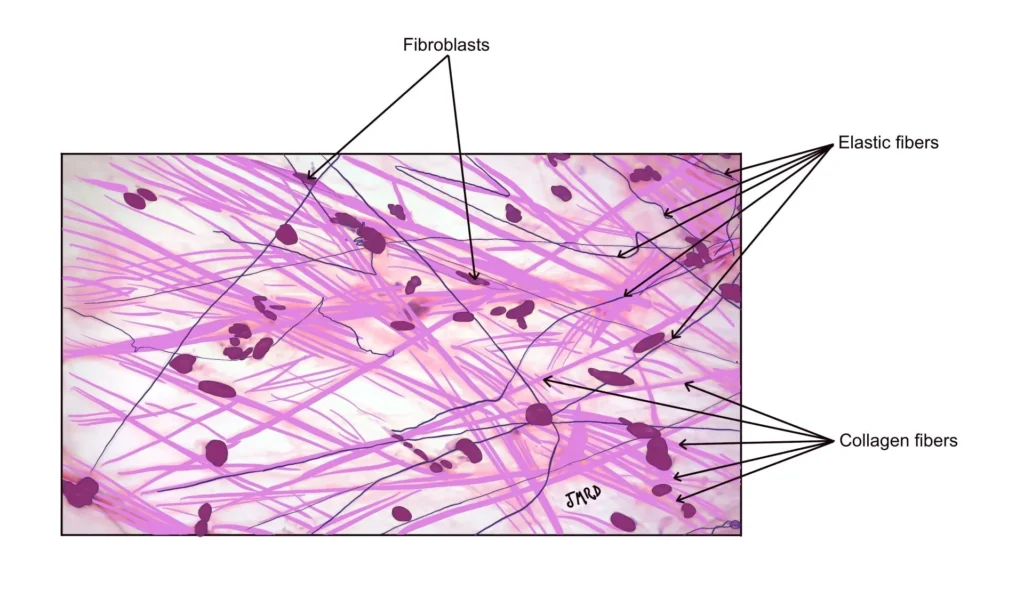
The loose arrangement of fibers allows for the diffusion of nutrients, oxygen, and waste products between blood vessels and surrounding tissues. For example, adipose tissue not only stores energy in the form of lipids but also acts as a thermal insulator, helping to maintain body temperature. Additionally, loose connective tissue houses immune cells, such as macrophages and mast cells, which play a critical role in defending the body against pathogens and aiding in wound healing.
Dense Connective Tissue
Dense connective tissue is characterized by a high density of collagen fibers, providing exceptional strength and resistance to mechanical stress. It is divided into two subtypes: dense regular connective tissue and dense irregular connective tissue, based on the orientation of its fibers.
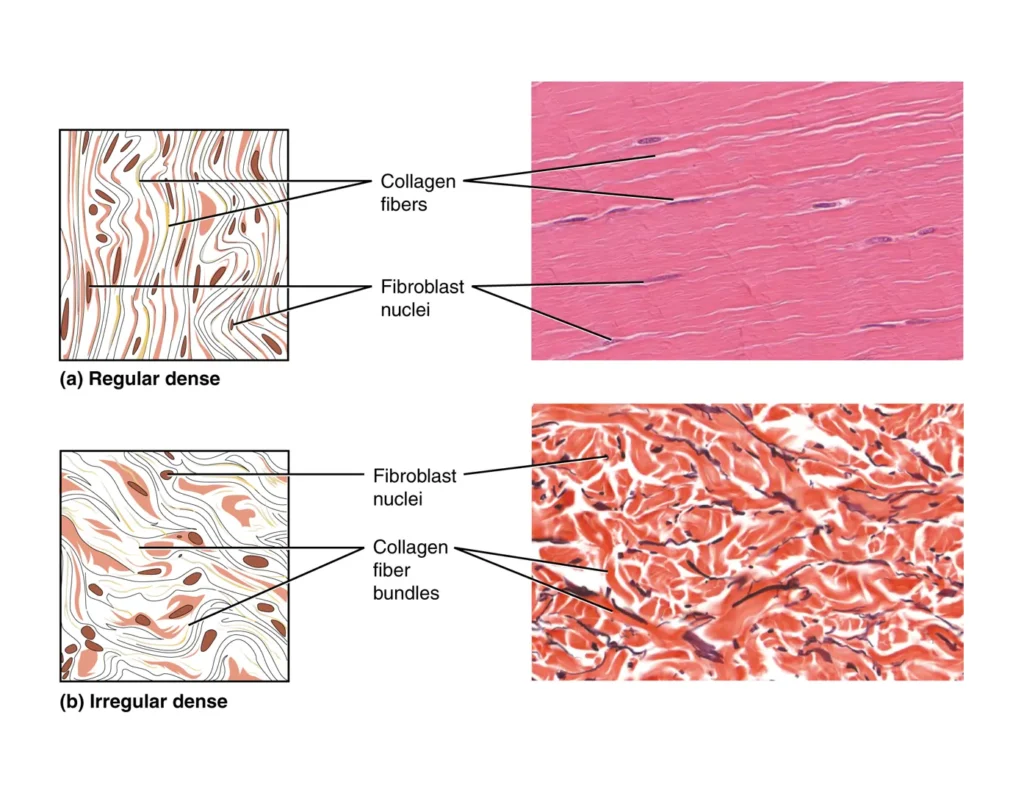
- Dense regular connective tissue features collagen fibers arranged in parallel, offering strength in a specific direction. This type is found in tendons, which connect muscles to bones, and ligaments, which link bones to bones, providing stability to joints. For instance, the Achilles tendon, which connects the calf muscle to the heel bone, is a prime example of dense regular connective tissue, enabling powerful movements like running and jumping.
- Dense irregular connective tissue has collagen fibers arranged in multiple directions, allowing it to withstand stress from various angles. This type is found in the dermis of the skin, organ capsules, and fibrous sheaths surrounding bones. Its multidirectional strength makes it ideal for areas subjected to complex mechanical forces, such as the skin, which must resist stretching and tearing.
Dense connective tissue is critical for maintaining the structural integrity of the body, protecting organs, and facilitating movement by anchoring muscles and bones.
Specialized Connective Tissue
Specialized connective tissue encompasses tissues with unique functions beyond basic support and connection. These include cartilage, bone, blood, and lymphoid tissue, each with distinct structural and functional properties.
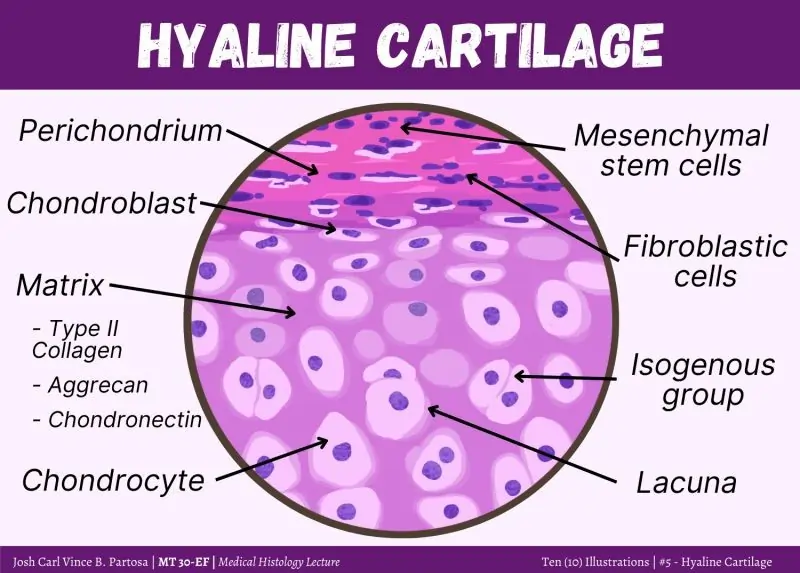
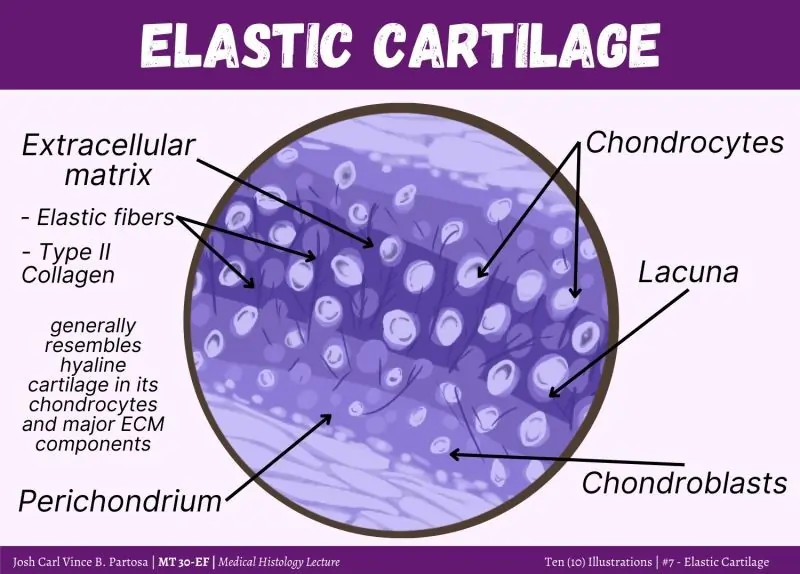
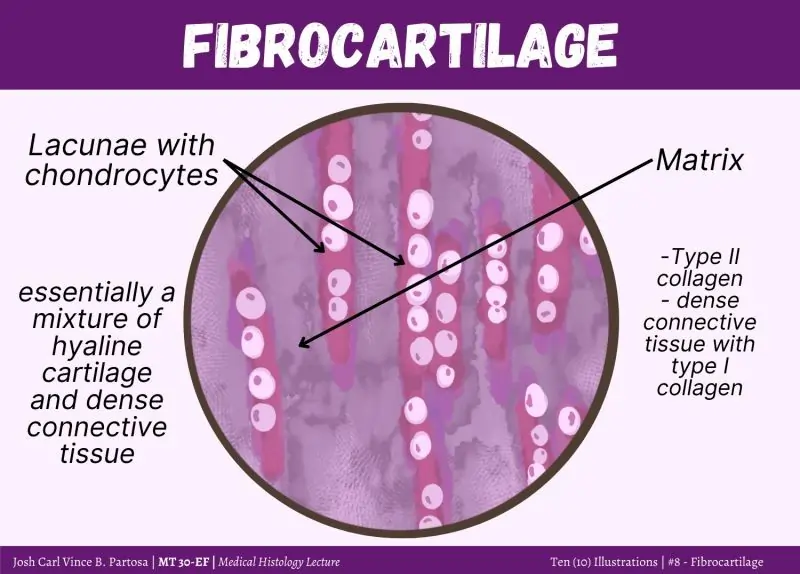
- Cartilage: This flexible yet firm tissue resists compression and provides support in areas like the nose, ears, and joints. Chondrocytes, the cells of cartilage, reside in small cavities called lacunae within a matrix rich in collagen and elastin. There are three types of cartilage: hyaline cartilage (found in the nose and trachea), elastic cartilage (in the ear), and fibrocartilage (in intervertebral discs), each tailored to specific mechanical demands.
- Bone: A hard, mineralized tissue, bone provides the body’s primary structural framework. Its matrix, rich in calcium salts and collagen, houses osteocytes in lacunae. Bones support soft tissues, protect vital organs, and enable movement by interacting with skeletal muscles. Additionally, red bone marrow within certain bones produces blood cells, a process known as hematopoiesis.
- Blood: As a fluid connective tissue, blood consists of plasma, red blood cells, white blood cells, and platelets. It serves as the body’s transport system, delivering oxygen, nutrients, and hormones while removing waste products. Blood also plays a key role in immune defense, with white blood cells combating infections.
- Lymphoid tissue: Found in lymph nodes, spleen, and bone marrow, lymphoid tissue supports immune functions by housing lymphocytes and other immune cells. It is critical for mounting immune responses against pathogens.
Specialized connective tissues perform highly specific roles, from providing structural support and flexibility to facilitating transport and immune defense.
Functions of Connective Tissue
Connective tissue performs a wide array of functions essential for the body’s structure, function, and survival. These functions are enabled by the diverse properties of its cells, fibers, and extracellular matrix. Below are the key functions of connective tissue:
- Support and Structure: Connective tissues, such as bones and ligaments, form the body’s structural framework, maintaining its shape and supporting organs. For example, the skeletal system provides a rigid framework for the body, while cartilage supports flexible structures like the trachea.
- Connection: Tissues like tendons and fascia bind different tissues together, ensuring a cohesive internal environment. Tendons, for instance, anchor muscles to bones, enabling coordinated movement.
- Protection: Connective tissues shield delicate organs from mechanical damage. The skull, a bony structure, protects the brain, while cartilage cushions joints to prevent friction-related injuries.
- Storage: Adipose tissue stores energy in the form of lipids, while bones store minerals like calcium and phosphorus. These reserves can be mobilized when needed, such as during pregnancy or bone remodeling.
- Transport: Blood, a specialized connective tissue, transports oxygen, nutrients, hormones, and waste products throughout the body, ensuring cellular function and homeostasis.
- Insulation: Adipose tissue acts as a thermal insulator, reducing heat loss and maintaining body temperature, particularly in cold environments.
- Cushioning: Cartilage and loose connective tissue absorb shock, protecting joints and organs from mechanical stress. For example, fibrocartilage in intervertebral discs cushions the spine during movement.
- Immune Response: Connective tissues, particularly lymphoid tissue, house immune cells that defend against pathogens and foreign substances. Macrophages in loose connective tissue engulf debris and pathogens, while lymphocytes in lymphoid tissue orchestrate immune responses.
- Repair and Regeneration: Connective tissues facilitate wound healing by providing a scaffold for cell migration and tissue remodeling. Fibroblasts produce collagen to repair damaged tissues, restoring structural integrity.
- Blood Cell Production: Red bone marrow within certain bones produces red blood cells, white blood cells, and platelets, essential for oxygen transport, immune defense, and blood clotting.
These functions highlight the versatility of connective tissue, making it indispensable for maintaining the body’s structural and physiological integrity.
Examples of Connective Tissue
Connective tissues are diverse, with each type adapted to specific roles. Below are key examples, categorized by type, along with their locations and functions:
| Type | Example | Location | Function |
|---|---|---|---|
| Loose Connective Tissue | Areolar tissue | Beneath the skin, around organs | Provides support, flexibility, and space for nutrient diffusion |
| Adipose tissue | Subcutaneous layer, around organs | Stores energy, insulates, cushions organs | |
| Dense Connective Tissue | Tendons | Between muscles and bones | Transmits mechanical force, enables movement |
| Ligaments | Between bones | Stabilizes joints, resists stress | |
| Fascia | Surrounding muscles and organs | Provides structural support, maintains shape | |
| Specialized Connective Tissue | Hyaline cartilage | Nose, trachea, ends of long bones | Provides smooth surfaces for joints, supports flexible structures |
| Elastic cartilage | Outer ear, epiglottis | Offers flexibility and resilience | |
| Fibrocartilage | Intervertebral discs, pubic symphysis | Absorbs shock, resists compression | |
| Bone | Skeleton | Provides structural support, protects organs, stores minerals | |
| Blood | Circulatory system | Transports oxygen, nutrients, and immune cells |
These examples illustrate the diversity of connective tissue, each tailored to specific anatomical and functional needs.
Connective Tissue Disorders
Disorders of connective tissue can significantly impact health, as they affect the body’s structural and functional integrity. These disorders may arise from genetic mutations, autoimmune reactions, or environmental factors. Below are some common connective tissue disorders:
- Rheumatoid Arthritis: An autoimmune disorder where the immune system attacks joint tissues, causing inflammation, pain, and joint damage. It primarily affects the synovial membranes but can also involve connective tissues in other organs.
- Systemic Lupus Erythematosus (SLE): This autoimmune condition affects multiple organs, including the skin, joints, kidneys, and heart. It causes inflammation and damage to connective tissues, leading to symptoms like joint pain, rashes, and fatigue.
- Scleroderma: Characterized by excessive collagen deposition, scleroderma leads to thickening and hardening of the skin and connective tissues in organs. It can cause vascular complications and organ dysfunction.
- Marfan Syndrome: A genetic disorder affecting the protein fibrillin, which is essential for connective tissue strength. It results in skeletal abnormalities (e.g., long limbs), cardiovascular issues (e.g., aortic aneurysms), and eye problems (e.g., lens dislocation).
- Ehlers-Danlos Syndrome (EDS): A group of genetic disorders caused by defective collagen production. EDS leads to hypermobile joints, fragile skin, and increased risk of organ rupture. There are multiple subtypes, each with varying severity.
- Osteogenesis Imperfecta: Also known as brittle bone disease, this genetic disorder affects collagen production in bones, leading to frequent fractures, bone deformities, and short stature.
These disorders underscore the importance of healthy connective tissue for maintaining bodily functions. Diagnosis often involves genetic testing, imaging, or biopsies, while treatment may include medications, physical therapy, or surgery, depending on the condition.
Additional Insights into Connective Tissue
Recent research has shed light on the dynamic roles of connective tissue beyond its traditional functions. For instance, the extracellular matrix is not merely a passive scaffold but an active participant in cellular communication. Matrix metalloproteinases (MMPs), enzymes produced by connective tissue cells, regulate matrix remodeling, influencing processes like tissue repair and cancer progression. Dysregulation of MMPs is implicated in conditions like arthritis and fibrosis, highlighting the matrix’s role in disease.
Moreover, connective tissue plays a critical role in mechanotransduction, the process by which mechanical forces are converted into biochemical signals. For example, the collagen fibers in tendons sense mechanical stress during movement, triggering cellular responses that maintain tissue health. This process is vital for adapting to physical activity and preventing injuries.
Connective tissue also interacts closely with the immune system. Adipose tissue, for instance, secretes signaling molecules called adipokines, which regulate inflammation and metabolism. In obesity, excessive adipose tissue can lead to chronic inflammation, contributing to diseases like diabetes and cardiovascular disorders. Similarly, lymphoid tissue in the spleen and lymph nodes orchestrates immune responses, making connective tissue a key player in immunity.
Conclusion
Connective tissue is the body’s unsung hero, providing the structural and functional support that enables life. From the flexible cartilage in joints to the fluid matrix of blood, connective tissue’s diversity is matched only by its indispensability. Its extracellular matrix and specialized cells work in harmony to support, protect, and connect the body’s tissues and organs. By facilitating transport, storing energy, and mounting immune defenses, connective tissue ensures the body’s resilience and adaptability.
Understanding the types, functions, and disorders of connective tissue reveals its critical role in health and disease. Disorders like Marfan syndrome and rheumatoid arthritis highlight the consequences of connective tissue dysfunction, emphasizing the need for continued research and therapeutic advancements. As science uncovers the dynamic roles of connective tissue in mechanotransduction, immune regulation, and tissue remodeling, its significance in medicine and biology continues to grow, solidifying its status as the body’s essential framework.
Frequently Asked Questions (FAQs)
FAQ 1: What is connective tissue, and why is it important in the body?
Connective tissue is one of the four primary tissue types in the body, alongside epithelial, muscle, and nervous tissues. It is defined by its extracellular matrix, a complex network of protein fibers, such as collagen and elastin, embedded in a gel-like ground substance. This matrix, secreted by specialized cells like fibroblasts, adipocytes, and immune cells, provides strength, elasticity, and resilience, enabling connective tissue to support, bind, and separate other tissues and organs. Connective tissue is found throughout the body, from the tendons connecting muscles to bones to the blood circulating nutrients, making it essential for structural integrity and physiological functions.
The importance of connective tissue lies in its diverse roles. It provides structural support, as seen in bones forming the skeleton, and connects tissues, such as ligaments stabilizing joints. Connective tissue also facilitates transport, with blood delivering oxygen and nutrients, and offers protection, like cartilage cushioning joints. Additionally, it contributes to energy storage in adipose tissue, insulation for temperature regulation, and immune defense through lymphoid tissue. For example, areolar tissue beneath the skin supports nutrient diffusion, while red bone marrow in bones produces blood cells, illustrating connective tissue’s critical role in maintaining homeostasis and overall health.
FAQ 2: What are the main types of connective tissue?
Connective tissue is categorized into three main types: loose connective tissue, dense connective tissue, and specialized connective tissue, each with distinct structures and functions. These types are determined by the composition and arrangement of their extracellular matrix and cells, allowing them to perform specific roles in the body.
- Loose connective tissue: This type features a loosely arranged network of collagen and elastin fibers in a gel-like matrix, providing flexibility and cushioning. Areolar tissue, found beneath the skin, supports organs and facilitates nutrient diffusion, while adipose tissue stores fat for energy and insulation, commonly located in the subcutaneous layer.
- Dense connective tissue: Characterized by tightly packed collagen fibers, this type offers strength and resistance to stress. Dense regular connective tissue, found in tendons and ligaments, has parallel fibers for unidirectional strength, while dense irregular connective tissue, in the dermis, has fibers in multiple directions for multidirectional resistance.
- Specialized connective tissue: This category includes cartilage, bone, blood, and lymphoid tissue. Cartilage, such as hyaline cartilage in the nose, resists compression, while bones provide structural support. Blood transports substances, and lymphoid tissue supports immune functions.
Each type is tailored to specific anatomical needs, ensuring the body’s structural and functional integrity. For instance, the Achilles tendon (dense regular) enables running, while elastic cartilage in the ear provides flexibility.
FAQ 3: What are the key functions of connective tissue?
Connective tissue performs a wide range of functions essential for the body’s structure, function, and survival, driven by its diverse cells, fibers, and extracellular matrix. These functions support nearly every physiological process, from movement to immune defense.
Key functions include:
- Support and structure: Connective tissues like bones and ligaments form the body’s framework, maintaining shape and supporting organs. The skeleton, for example, supports soft tissues.
- Connection: Tissues such as tendons and fascia bind muscles to bones and organs to each other, ensuring a cohesive internal environment.
- Protection: Bones protect vital organs (e.g., the skull shields the brain), while cartilage cushions joints to prevent friction.
- Storage: Adipose tissue stores energy as lipids, and bones store minerals like calcium for metabolic needs.
- Transport: Blood, a fluid connective tissue, delivers oxygen, nutrients, and hormones while removing waste.
- Insulation: Adipose tissue reduces heat loss, maintaining body temperature.
- Immune response: Lymphoid tissue in lymph nodes houses immune cells, combating pathogens.
- Repair and regeneration: Fibroblasts produce collagen for wound healing, restoring tissue integrity.
- Blood cell production: Red bone marrow produces blood cells, essential for oxygen transport and immunity.
For example, cartilage in the knee absorbs shock during running, while blood transports oxygen to muscles, highlighting connective tissue’s multifaceted contributions to health.
FAQ 4: What are some examples of connective tissue in the body?
Connective tissue exists in various forms, each adapted to specific roles based on its structure and location. These examples illustrate the diversity of connective tissue and its critical functions across the body.
- Loose connective tissue: Areolar tissue, found beneath the skin and around organs, provides support and flexibility, acting as a packing material. Adipose tissue, located in the subcutaneous layer and around organs like the kidneys, stores energy, insulates, and cushions.
- Dense connective tissue: Tendons, such as the Achilles tendon, connect muscles to bones, enabling movement. Ligaments, like those in the knee, stabilize joints. Fascia, surrounding muscles, provides structural support and maintains shape.
- Specialized connective tissue: Hyaline cartilage in the nose and trachea supports flexible structures, while elastic cartilage in the ear offers resilience. Fibrocartilage in intervertebral discs absorbs shock. Bone forms the skeleton, protecting organs and enabling movement. Blood, with its plasma and cells, transports oxygen and nutrients. Lymphoid tissue in the spleen supports immune functions.
These examples demonstrate how connective tissue’s versatility ensures the body’s structural integrity and functionality. For instance, adipose tissue insulates during cold weather, while tendons facilitate athletic performance.
FAQ 5: How does loose connective tissue differ from dense connective tissue?
Loose connective tissue and dense connective tissue differ in their structure, fiber arrangement, and functions, reflecting their distinct roles in the body. These differences arise from the composition of their extracellular matrix and the density of fibers.
Loose connective tissue has a loosely arranged network of collagen and elastin fibers in a gel-like matrix, providing flexibility and cushioning. It is found beneath the skin, around blood vessels, and in mucous membranes. Subtypes include areolar tissue, which supports nutrient diffusion, and adipose tissue, which stores fat and insulates. Its loose structure allows for the presence of immune cells like macrophages, aiding in defense and wound healing. For example, areolar tissue beneath the skin facilitates nutrient exchange between blood and tissues.
In contrast, dense connective tissue is characterized by tightly packed collagen fibers, offering strength and resistance to mechanical stress. It includes dense regular connective tissue, with parallel fibers in tendons and ligaments, and dense irregular connective tissue, with multidirectional fibers in the dermis and organ capsules. Dense regular tissue, like the patellar ligament, withstands unidirectional stress, while dense irregular tissue in the skin resists stretching in multiple directions. Its high fiber density limits flexibility but enhances durability.
These structural differences determine their functions: loose connective tissue prioritizes flexibility and support, while dense connective tissue focuses on strength and stability, ensuring the body’s diverse mechanical needs are met.
FAQ 6: What role does the extracellular matrix play in connective tissue?
The extracellular matrix is the defining feature of connective tissue, consisting of protein fibers (collagen, elastin) and a gel-like ground substance secreted by cells like fibroblasts. It provides the structural and functional foundation for connective tissue’s diverse roles, distinguishing it from other tissue types.
The extracellular matrix determines the tissue’s mechanical properties. Collagen fibers provide tensile strength, as seen in tendons, while elastin fibers confer elasticity, allowing tissues like ligaments to stretch and recoil. The ground substance, composed of water, glycosaminoglycans, and proteoglycans, acts as a medium for nutrient diffusion and resists compression, as in cartilage. This matrix supports cells, such as chondrocytes in cartilage or osteocytes in bone, housed in small cavities called lacunae.
Beyond structure, the matrix plays dynamic roles. It facilitates mechanotransduction, converting mechanical forces into biochemical signals, as in tendons during movement. It also regulates cellular behavior, influencing processes like wound healing and tissue remodeling through enzymes like matrix metalloproteinases (MMPs). For example, in areolar tissue, the matrix allows nutrient exchange between blood and tissues, while in bone, it stores calcium for metabolic needs. The extracellular matrix’s versatility ensures connective tissue’s ability to support, protect, and maintain bodily functions.
FAQ 7: What are common connective tissue disorders?
Connective tissue disorders affect the structural and functional integrity of tissues like cartilage, bone, and blood, often resulting from genetic mutations, autoimmune reactions, or environmental factors. These conditions can significantly impact quality of life, affecting multiple organ systems.
- Rheumatoid arthritis: An autoimmune disorder where the immune system attacks joint tissues, causing inflammation, pain, and joint damage. It affects connective tissues in the synovial membranes and can involve other organs.
- Systemic lupus erythematosus (SLE): This autoimmune condition targets multiple tissues, including skin, joints, and kidneys, leading to inflammation and damage. Symptoms include joint pain, rashes, and fatigue.
- Scleroderma: Characterized by excessive collagen deposition, it causes thickening and hardening of the skin and organs, leading to vascular and organ complications.
- Marfan syndrome: A genetic disorder affecting fibrillin, resulting in skeletal abnormalities (e.g., long limbs), cardiovascular issues (e.g., aortic aneurysms), and eye problems.
- Ehlers-Danlos syndrome (EDS): A group of genetic disorders due to defective collagen, causing joint hypermobility, fragile skin, and organ rupture risks.
- Osteogenesis imperfecta: A genetic condition causing brittle bones due to collagen defects, leading to frequent fractures and deformities.
Diagnosis involves genetic testing, imaging, or biopsies, while treatments include medications, physical therapy, or surgery. For example, rheumatoid arthritis may be managed with anti-inflammatory drugs, highlighting the need for targeted therapies to address connective tissue damage.
FAQ 8: How does connective tissue contribute to immune defense?
Connective tissue plays a vital role in the body’s immune defense, serving as a physical and functional platform for immune activity. Its cells and structures, particularly lymphoid tissue and immune cells within loose connective tissue, are integral to combating pathogens and maintaining immune homeostasis.
Loose connective tissue, such as areolar tissue, contains immune cells like macrophages, mast cells, and plasma cells. Macrophages engulf pathogens and debris, initiating immune responses, while mast cells release histamine to trigger inflammation, alerting the immune system to infections. For example, in a skin abrasion, macrophages in the subcutaneous tissue clear bacteria, preventing infection.
Lymphoid tissue, found in lymph nodes, and spleen, is specialized for immune functions. It houses lymphocytes, including B cells and T cells, which orchestrate targeted responses. Lymph nodes filter lymph, trapping pathogens for immune processing, while the spleen removes damaged blood cells and pathogens from circulation. For instance, during a viral infection, lymph nodes swell as lymphocytes proliferate to combat the virus.
Additionally, the extracellular matrix of connective tissue supports immune cell migration during inflammation, facilitating rapid responses to injury. Adipose tissue secretes adipokines, regulating inflammation, though excess adipose tissue can lead to chronic inflammation in obesity. These mechanisms demonstrate connective tissue integrates structural support with immune defense, ensuring effective immune responses.
FAQ 9: How does connective tissue function beyond fat storage?
While adipose tissue is widely known for fat storage, its functions extend far beyond energy storage, making it a dynamic and multifunctional connective tissue. As a subtype of loose connective tissue, adipose tissue performs critical roles in insulation, protection, and metabolic regulation, influencing overall health.
- Insulation: Adipose tissue, found in the subcutaneous layer, acts as a thermal insulator, reducing heat loss and maintaining body temperature, particularly in cold environments. For example, it helps individuals adapt to cold climates.
- Cushioning: It protects organs like the kidneys and heart by cushioning them against mechanical stress, absorbing shock during movement.
- Metabolic regulation: Adipose tissue secretes signaling molecules called adipokines, such as leptin, which regulate inflammation and metabolism. These regulate appetite, insulin sensitivity, and immune responses. In obesity, dysregulated adipokine** production can contribute to chronic inflammation and diseases like type diabetes2 diabetes.
- Endocrine function: Adipose tissue acts as an an endocrine organ, releasing hormones that influence energy balance and glucose metabolism, impacting metabolic health.
For instance, during prolonged fasting, adipose tissue mobilizes stored lipids to provide energy for vital organs. Its role in inflammation regulation **is critical, as excessive adipose tissue in obesity can exacerbate conditions like **atherosclerosis. These diverse functions highlight adipose tissue’s importance beyond mere fat storage, underscoring its role in physiological homeostasis.
FAQ 10: How does connective tissue support joint health?
Connective tissue is critical for maintaining joint health, providing the structural support, flexibility, and stability needed for movement while preventing injury. Cartilage, tendons, ligaments, and synovial tissue within joints are key connective tissues that ensure joint functionality and resilience.
- Cartilage: Hyaline cartilage covers articular surfaces in joints like the knee, providing a smooth surface for low-friction movement and reducing friction between bones. Fibrocartilage, found in intervertebral discs and the meniscus, absorbs shock, cushioning joints during high-impact activities like running.
- Tendons: These connect muscles to bones, transmitting forces to enable joint movement. For example, the patellar tendon facilitates knee extension during walking.
- Ligaments: These stabilize joints by connecting bones, preventing excessive movement. The anterior cruciate ligament (ACL) in the knee ensures stability during pivoting motions.
- Synovial tissue: This connective tissue produces synovial fluid, which lubricates joints, reducing friction and nourishing cartilage, found in cartilage.
The extracellular matrix in these tissues, rich in collagen and elastin, provides strength and elasticity, while chondrocytes in cartilage maintain matrix integrity. Damage to these tissues, as in osteoarthritis, leads to joint pain and stiffness due to cartilage degradation. Regular exercise and a balanced diet rich in collagen-supporting nutrients, like vitamin C, support joint health by promoting tissue repair and maintenance, underscoring connective tissue’s essential role in mobility and joint function.
FAQ 11: How does connective tissue contribute to wound healing?
Connective tissue plays a pivotal role in wound healing, orchestrating the repair and regeneration of damaged tissues through its specialized cells and extracellular matrix. This process involves multiple stages, including hemostasis, inflammation, proliferation, and remodeling, with connective tissue contributing significantly to each phase. Fibroblasts, macrophages, and the matrix itself are key players in restoring tissue integrity after injury.
During the initial inflammatory phase, loose connective tissue, such as areolar tissue, facilitates immune responses. Macrophages clear debris and pathogens, while mast cells release signaling molecules to attract immune cells. In the proliferation phase, fibroblasts in the connective tissue produce collagen and other matrix components, forming a temporary scaffold called granulation tissue. This scaffold supports cell migration and new blood vessel formation, as seen in skin wounds. In the remodeling phase, the extracellular matrix is reorganized, with matrix metalloproteinases (MMPs) refining collagen alignment for strength, transforming granulation tissue into a mature scar.
For example, in a deep cut, fibroblasts in the dermis (dense irregular connective tissue) deposit collagen to close the wound, while blood (a specialized connective tissue) delivers nutrients and oxygen. Dysregulated healing, as in keloid scars, can result from excessive collagen production, highlighting the need for balanced connective tissue activity. This intricate process underscores connective tissue’s essential role in tissue repair and regeneration.
FAQ 12: What is the role of cartilage in connective tissue functions?
Cartilage, a specialized connective tissue, is critical for providing support, flexibility, and shock absorption in various parts of the body. Its unique structure, characterized by a firm yet flexible extracellular matrix rich in collagen and elastin, allows it to withstand compressive forces while maintaining resilience. Chondrocytes, the primary cells of cartilage, reside in small cavities called lacunae, maintaining the matrix’s integrity.
Cartilage serves multiple functions:
- Support: Hyaline cartilage in the trachea keeps airways open, while elastic cartilage in the ear maintains shape with flexibility.
- Shock absorption: Fibrocartilage in intervertebral discs and the knee meniscus cushions joints, protecting bones during movement.
- Smooth movement: Hyaline cartilage covers articular surfaces in joints, reducing friction, as seen in the hip joint during walking.
- Growth and development: In embryos, cartilage serves as a precursor to bone in endochondral ossification, forming long bones like the femur.
Unlike other connective tissues, cartilage lacks blood vessels, relying on diffusion through the matrix for nutrient delivery, which slows healing after injury. For instance, a torn meniscus (fibrocartilage) often requires surgical intervention due to poor regenerative capacity. Cartilage’s contributions to joint health and structural support make it indispensable for mobility and skeletal integrity.
FAQ 13: How does bone function as a connective tissue?
Bone, a specialized connective tissue, is the body’s primary structural framework, providing support, protection, and mobility. Its hard, mineralized extracellular matrix, rich in calcium salts and collagen, gives bone its strength and rigidity. Osteocytes, the primary cells, reside in lacunae, communicating through tiny channels to maintain bone health. Bone’s unique properties make it a dynamic tissue with multiple functions beyond structural support.
Key functions include:
- Structural support: Bones form the skeleton, supporting soft tissues and maintaining body shape, as seen in the vertebral column supporting the torso.
- Protection: Bones shield vital organs, such as the skull protecting the brain and the ribcage safeguarding the heart.
- Movement: Bones interact with skeletal muscles via tendons, enabling movement, like the humerus facilitating arm motion.
- Mineral storage: Bones store calcium and phosphorus, releasing them for metabolic needs, such as muscle contraction.
- Blood cell production: Red bone marrow in flat bones like the sternum produces red blood cells, white blood cells, and platelets through hematopoiesis.
Bone is constantly remodeled by osteoblasts (bone-forming cells) and osteoclasts (bone-resorbing cells), ensuring strength and adaptability. For example, weight-bearing exercise strengthens bones by stimulating osteoblast activity. Conditions like osteoporosis, where bone density decreases, highlight bone’s critical role in maintaining structural integrity and overall health.
FAQ 14: Why is blood considered a connective tissue?
Blood is classified as a specialized connective tissue due to its extracellular matrix and role in connecting and supporting bodily functions, despite its fluid nature. Unlike other connective tissues with solid matrices, blood’s matrix is plasma, a liquid containing water, proteins, and electrolytes. Suspended within plasma are red blood cells, white blood cells, and platelets, which function as the cellular components, analogous to fibroblasts or chondrocytes in other connective tissues.
Blood’s connective tissue characteristics include:
- Transport: Blood delivers oxygen, nutrients, and hormones to tissues and removes waste products like carbon dioxide, as seen in oxygen transport from lungs to muscles.
- Immune defense: White blood cells, such as lymphocytes, combat infections, protecting the body from pathogens.
- Clotting: Platelets initiate blood clotting to prevent excessive bleeding, as in a cut.
- Homeostasis: Blood regulates body temperature, pH, and fluid balance, ensuring physiological stability.
For example, during exercise, blood transports oxygen to working muscles and removes lactic acid, supporting metabolic demands. Blood’s origin from mesenchyme, the embryonic tissue giving rise to all connective tissues, further supports its classification. Its role in connecting distant tissues and maintaining systemic functions underscores its status as a vital connective tissue.
FAQ 15: How does connective tissue support metabolic processes?
Connective tissue supports metabolic processes by facilitating nutrient storage, transport, and regulation, ensuring the body’s energy and biochemical needs are met. Its diverse types, including adipose tissue, blood, and bone, contribute to metabolism through their specialized structures and functions.
- Energy storage: Adipose tissue stores lipids as an energy reserve, releasing them during fasting or high energy demand, such as during prolonged exercise.
- Nutrient transport: Blood, a fluid connective tissue, delivers glucose, amino acids, and fatty acids to cells while removing metabolic waste, maintaining cellular function.
- Mineral regulation: Bone stores calcium and phosphorus, releasing them into the bloodstream for processes like muscle contraction and nerve signaling.
- Metabolic signaling: Adipose tissue secretes adipokines, such as leptin, which regulate appetite and insulin sensitivity, influencing glucose metabolism.
- Blood cell production: Red bone marrow produces red blood cells for oxygen transport, critical for cellular respiration.
For instance, in starvation, adipose tissue mobilizes lipids to fuel the body, while blood distributes these nutrients. Dysregulation, as in obesity, can lead to metabolic disorders like type 2 diabetes due to excessive adipokine production. Connective tissue’s role in metabolism highlights its importance in maintaining energy balance and physiological homeostasis.
FAQ 16: What is the significance of tendons and ligaments in connective tissue?
Tendons and ligaments, types of dense regular connective tissue, are critical for movement and joint stability, owing to their high collagen content and parallel fiber arrangement. These tissues withstand significant tensile forces, connecting different structures to ensure coordinated bodily functions. Their dense, organized structure distinguishes them from other connective tissues like loose connective tissue.
- Tendons: These connect skeletal muscles to bones, transmitting forces to enable movement. For example, the Achilles tendon facilitates plantar flexion during running.
- Ligaments: These connect bones to bones, stabilizing joints and preventing excessive motion. The anterior cruciate ligament (ACL) in the knee ensures stability during pivoting.
- Both tissues provide strength due to tightly packed collagen fibers, offering resistance to unidirectional stress.
- They have limited elasticity, ensuring efficient force transmission but making them prone to injuries like sprains or tears.
Tendons and ligaments are vital for physical activities, from walking to athletic performance. Injuries, such as a torn ACL, often require surgical repair due to poor vascularity, slowing natural healing. Their role in maintaining structural integrity and enabling mobility underscores their significance in the connective tissue system.
FAQ 17: How does connective tissue adapt to mechanical stress?
Connective tissue exhibits remarkable adaptability to mechanical stress, a process driven by mechanotransduction, where mechanical forces are converted into biochemical signals. This adaptability ensures tissues like tendons, bones, and cartilage maintain strength and functionality under varying physical demands, preventing injury and supporting movement.
- Bone remodeling: Osteoblasts and osteoclasts respond to stress, such as weight-bearing exercise, by depositing or removing bone matrix, increasing bone density. For example, runners develop stronger leg bones.
- Tendon strengthening: Fibroblasts in tendons produce more collagen under repetitive stress, enhancing tensile strength, as seen in athletes’ tendons.
- Cartilage maintenance: Chondrocytes adjust matrix production in response to compressive forces, maintaining joint cushioning, as in knee cartilage during walking.
- The extracellular matrix reorganizes under stress, with matrix metalloproteinases (MMPs) refining collagen alignment for durability.
This adaptability is critical for physical resilience. For instance, resistance training strengthens bones and tendons, reducing fracture risk. However, excessive stress, as in overuse injuries, can overwhelm adaptive mechanisms, leading to conditions like tendinitis. Connective tissue’s ability to adapt to mechanical stress ensures it meets the body’s dynamic structural needs.
FAQ 18: What are the challenges in treating connective tissue injuries?
Treating connective tissue injuries, such as those to cartilage, tendons, or ligaments, poses significant challenges due to their unique structural properties and limited regenerative capacity. These tissues often have poor vascularity and slow cellular turnover, complicating natural healing processes and requiring specialized interventions.
- Limited blood supply: Tissues like cartilage and tendons lack extensive blood vessels, slowing nutrient delivery and healing. For example, a torn meniscus often heals poorly without surgery.
- Slow cell turnover: Chondrocytes in cartilage and fibroblasts in tendons have low proliferation rates, delaying tissue repair compared to vascular tissues like skin.
- Scar tissue formation: Healing tendons or ligaments may form weaker scar tissue, reducing strength, as seen in rotator cuff injuries.
- Mechanical demands: Injured tissues must withstand stress during healing, complicating recovery. For instance, a repaired ACL requires gradual rehabilitation to restore stability.
Treatment strategies include physical therapy to restore function, surgical interventions like tendon grafts, or emerging therapies like platelet-rich plasma (PRP) to stimulate healing. Chronic conditions, such as osteoarthritis, result from cumulative cartilage damage, requiring joint replacements in severe cases. These challenges highlight the need for advanced regenerative medicine to improve connective tissue repair outcomes.
FAQ 19: How does connective tissue interact with the immune system?
Connective tissue interacts closely with the immune system, serving as a physical and functional platform for immune responses. Loose connective tissue, lymphoid tissue, and adipose tissue house immune cells and signaling molecules, facilitating pathogen defense and inflammation regulation, ensuring the body’s protection and homeostasis.
- Immune cell housing: Areolar tissue contains macrophages, mast cells, and lymphocytes, which initiate immune responses. Macrophages engulf pathogens, as in wound infections, while mast cells trigger inflammation.
- Lymphoid tissue: Found in lymph nodes and spleen, it supports B cells and T cells, orchestrating targeted immune responses. Lymph nodes filter pathogens, as during bacterial infections.
- Inflammation regulation: Adipose tissue secretes adipokines, modulating inflammation. In obesity, excessive adipokines contribute to chronic inflammation, increasing disease risk.
- Matrix support: The extracellular matrix facilitates immune cell migration during inflammation, aiding rapid responses, as in skin infections.
For example, during a viral infection, lymph nodes swell as lymphocytes proliferate, supported by lymphoid tissue’s connective framework. Dysregulated interactions, as in rheumatoid arthritis, lead to autoimmune attacks on connective tissues, causing joint damage. These interactions highlight connective tissue’s integral role in immune defense and systemic health.
FAQ 20: What are the emerging research areas in connective tissue biology?
Connective tissue biology is a rapidly evolving field, with emerging research uncovering novel roles and therapeutic potential for tissues like cartilage, bone, and adipose tissue. Advances in molecular biology, bioengineering, and regenerative medicine are driving insights into connective tissue’s dynamic functions, offering hope for treating related disorders.
Key research areas include:
- Regenerative medicine: Stem cell therapies aim to repair cartilage or tendons, as in osteoarthritis, by inducing tissue regeneration.
- Tissue engineering: Bioengineered scaffolds mimic the extracellular matrix, supporting tissue repair, such as 3D-printed bone grafts.
- Matrix dynamics: Studies of matrix metalloproteinases (MMPs) explore their role in tissue remodeling, with implications for wound healing and cancer.
- Adipose tissue signaling: Research on adipokines investigates their role in metabolism and inflammation, targeting obesity-related diseases like type 2 diabetes.
- Mechanotransduction: Understanding how mechanical forces influence connective tissue, as in bone remodeling, informs therapies for osteoporosis.
For example, cartilage regeneration using stem cells could reduce reliance on joint replacements, while adipokine-targeted drugs may treat metabolic disorders. These advances highlight connective tissue’s complexity and its potential as a therapeutic target, promising improved outcomes for structural and systemic health conditions.
Acknowledgement
The development of the article “Connective Tissue: The Essential Framework of the Body” was made possible through the comprehensive and reliable information provided by various reputable online sources. These platforms offered valuable insights into the structure, functions, types, and disorders of connective tissue, ensuring the article’s accuracy and depth. The Examsmeta.com website sincerely expresses its gratitude to the following websites for their contributions to this work:
- National Institute of Arthritis and Musculoskeletal and Skin Diseases: For detailed information on connective tissue disorders like rheumatoid arthritis and scleroderma.
- Cleveland Clinic: For clear explanations of connective tissue types and their roles in joint health.
- Mayo Clinic: For insights into connective tissue disorders such as Marfan syndrome and Ehlers-Danlos syndrome.
- WebMD: For accessible overviews of cartilage, bone, and blood as specialized connective tissues.
- Healthline: For comprehensive details on adipose tissue functions and metabolic roles.
- MedlinePlus: For reliable information on genetic connective tissue disorders and their symptoms.
- Johns Hopkins Medicine: For in-depth discussions on tendon and ligament injuries and treatments.
- PubMed: For access to peer-reviewed studies on extracellular matrix dynamics and mechanotransduction.
- ScienceDirect: For research articles on matrix metalloproteinases and tissue remodeling.
- Nature: For cutting-edge research on connective tissue biology and regenerative medicine.
- Harvard Health Publishing: For insights into bone remodeling and osteoporosis prevention.
- American Academy of Orthopaedic Surgeons: For detailed explanations of cartilage and joint function.
- British Society for Immunology: For information on lymphoid tissue and immune responses.
- Medical News Today: For accessible content on blood as a connective tissue and its functions.
- Stanford Medicine: For advanced research on adipose tissue signaling and adipokines.

